Introduction
Physical therapy in Duluth for Osteoarthritis of the Ankle
Welcome to In Motion Therapy's patient resource about Osteoarthritis of the Ankle.
Injuries of the ankle joint are common. While ankle fractures and ankle sprains heal pretty well, they can lead to problems much later in life. This is due to the wear and tear that occurs over the years after the injury. This condition is called osteoarthritis (OA) or posttraumatic arthritis. Trauma means injury, and the term posttraumatic arthritis is used to describe arthritis that develops after an injury.
This document will help you understand:
- how arthritis of the ankle develops
- how doctors diagnose the condition
- what treatment options are available
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Foot therapy|limit:15|heading:Hear from some of our *Foot Therapy* patients#
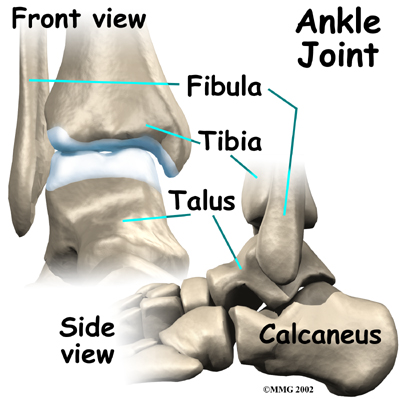
Anatomy
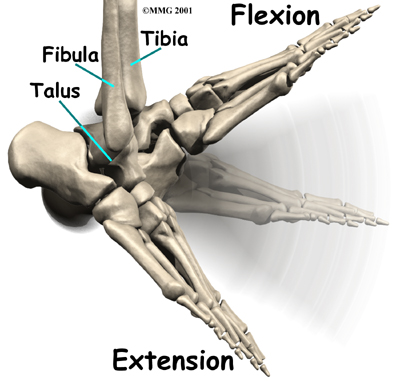
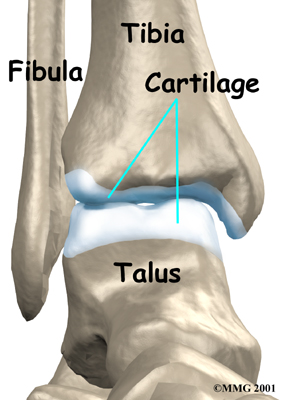
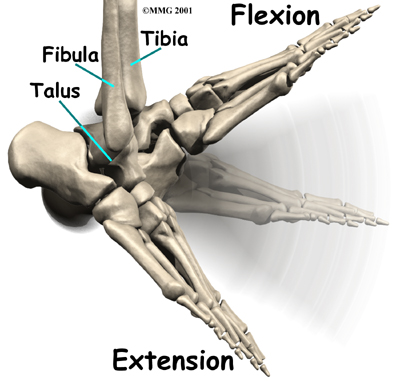
The ankle joint is made up of three bones: the lower end of the tibia (shinbone), the fibula (the small bone of the lower leg), and the talus (the bone that fits into the socket formed by the tibia and fibula).
The talus sits on top of the calcaneus (the heelbone). The talus moves mainly in one direction. It works like a hinge to allow your .
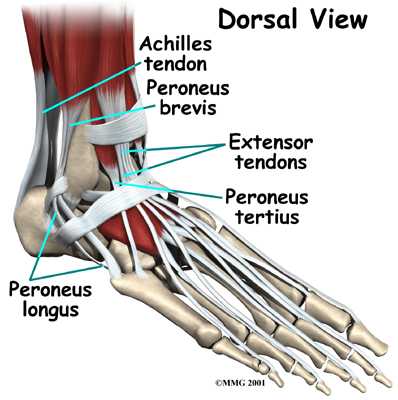
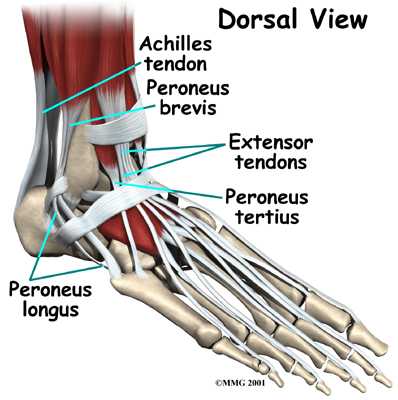
Ligaments on both sides of the ankle joint help hold the bones together. Many cross the ankle to move the ankle and the toes. (Ligaments connect bones to bones while tendons connect muscles to bones.) The large Achilles tendon in the back is the most powerful tendon in the foot. It connects the calf muscles to the heel bone and gives the foot the power for walking, running, and jumping.
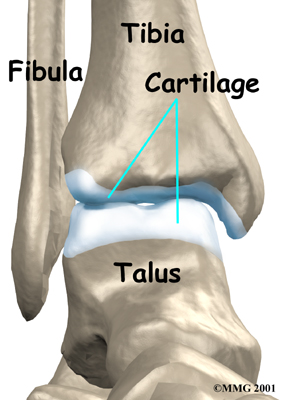
Inside the joint, the bones are covered with a slick, smooth material called . Articular cartilage is the material that allows the bones to move against one another in the joints of the body. The cartilage lining is about one-quarter of an inch thick in most joints that carry body weight, such as the ankle, hip, or knee. It is soft enough to allow for shock absorption but tough enough to last a lifetime, as long as it is not injured.
Related Article: In Motion Therapy's Guide to Ankle Anatomy
Causes
OA is usually considered a type of , or wear-and-tear arthritis. Doctors consider OA pretty much the same whether it appears years after an injury to the joint or whether it appears without any history of injury. It behaves more or less the same way.
Over the past several years, there has been increasing evidence that OA is genetic, meaning that it runs in families. OA that occurs without any injury may prove to be related to differences in the chemical makeup of articular cartilage. People are born with these differences.
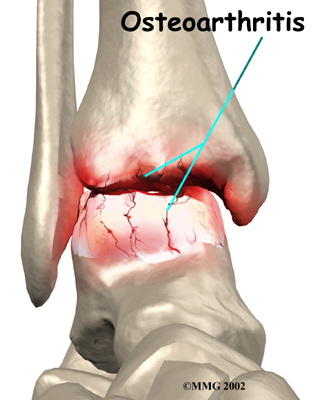
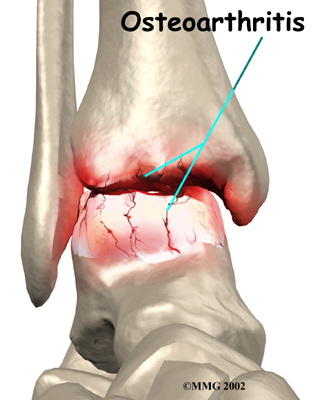
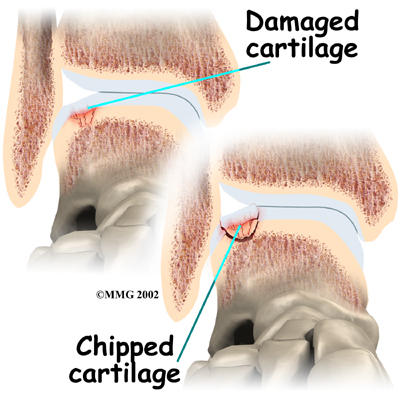
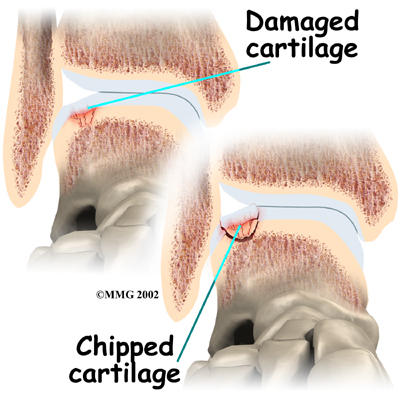 Injury to a joint, such as a bad sprain or fracture, can cause . The cartilage can be bruised when too much pressure is exerted on it. This damages the cartilage, although if you look at the surface it may not appear to be any different. The injury to the material doesn't show up until months later. Sometimes the cartilage surface is damaged even more severely, and pieces of the cartilage are ripped from the bone. These pieces do not heal back and usually must be removed from the joint surgically. If not, they may float around in the joint, causing the joint to catch and be painful. These fragments of cartilage may also do more damage to the joint surface.
Injury to a joint, such as a bad sprain or fracture, can cause . The cartilage can be bruised when too much pressure is exerted on it. This damages the cartilage, although if you look at the surface it may not appear to be any different. The injury to the material doesn't show up until months later. Sometimes the cartilage surface is damaged even more severely, and pieces of the cartilage are ripped from the bone. These pieces do not heal back and usually must be removed from the joint surgically. If not, they may float around in the joint, causing the joint to catch and be painful. These fragments of cartilage may also do more damage to the joint surface.
Once this cartilage is ripped away, it does not normally grow back. Unlike bone, holes in the surface are not simply replaced by the cartilage tissue around the hole. Instead the defects are filled with scar tissue. The scar tissue that forms is not nearly as good a material for covering joint surfaces as the cartilage it replaces. It just can't support weight and isn't smooth like true articular cartilage.
An injury to a joint, even if it does not injure the articular cartilage directly, can alter how the joint works. This is true for a fracture where the bone fragments heal differently from the way they were before the break occurred. It is also true when ligaments are damaged that lead to instability in the joint. When an injury results in a change in the way the joint moves, the injury may increase the forces on the articular cartilage. This is similar to any mechanical device or machinery. If the mechanism is out of balance, it wears out faster.
Over many years this imbalance in the joint mechanics can lead to damage to the articular surface. Since articular cartilage cannot heal itself very well, the damage adds up. Finally, the joint is no longer able to compensate for the increasing damage, and it begins to hurt. The damage occurs well before the pain begins.
In summary, arthritis may come from differences in how each of us is put together based on our genes, a condition best described as OA. Or arthritis may develop years after an injury that leads to slow damage to the joint surfaces, a condition probably best described as post-traumatic arthritis. Either way the joint is worn out, and it hurts. For the purposes of this document, we will refer to both types as OA.
Symptoms
Pain is the main problem with arthritis of any joint. This pain occurs at first only related to activity. Usually, once the activity gets underway there is not much pain, but after resting for several minutes the pain and stiffness increase. Later, when the condition worsens, pain may be present even at rest. The pain may interfere with sleep. The joint may swell, fill with fluid, and feel tight, especially following increased activity. As the articular cartilage starts to wear off the joint surface, the joint may squeak when moved. Doctors refer to this sound as crepitation.
OA will eventually affect the motion of a joint. The joint becomes stiff and loses flexibility. Certain movements can become painful, and it may become difficult to trust the joint to hold your weight in certain positions. The body has a pain reflex such that when a joint is put into a position that causes pain the muscles around the joint may stop working without warning. This reflex can cause a person to stumble or even fall when arthritis affects the ankle joint.
When OA has reached a very severe stage, the bone itself under the articular cartilage may become worn away. This can lead to increasing deformities around the joint. In the final stages, the alignment of the bones can begin to form odd angles where they meet at the joint.
Diagnosis
The diagnosis of OA begins with a history of the problem. Details about any injuries that may have occurred to the joint, even years before, are important in helping up understand why the condition exists. Whether or not other family members have OA may also shed some light on the problem.
Following the history, the physical therapists at In Motion Therapy will examine the ankle joint and possibly other joints in your body. It will be important for us to see how the motion of the ankle has been affected. The alignment of the ankle will be assessed. The nerves and circulation going to the legs and ankle will be checked. Your therapist will watch you walk to see if you have a noticeable limp.
Our physical therapist may also refer you to a doctor for X-rays or other diagnostic tools that can aid in obtaining an accurate diagnosis, prior to the start of your physical therapy program.
Our Treatment
What can be done for the condition?
The treatment of OA of the ankle can be divided into the nonsurgical means to control the symptoms and the surgical procedures that are available to treat the condition. Surgery is usually not considered until it has become impossible to control the symptoms without it.
Non-surgical Rehabilitation
Rehabilitation services, such as those offered at In Motion Therapy, play a critical role in the treatment plan for ankle joint arthritis. Treatment usually begins when the ankle first becomes painful. The pain may only occur at first with heavy use and may simply require the use of mild anti-inflammatory medications such as aspirin or ibuprofen. Reducing the activity or changing from occupations that require long periods of standing and walking may be necessary to help control the symptoms.
The main goal of your physical therapy program is to help you learn how to control symptoms and maximize the health of your ankle. Our therapist will instruct you on techniques you can use to calm your pain and symptoms. We may advise may use rest, heat, or topical rubs. Our physical therapist will work with you to improve flexibility, balance, and strength. Our physical therapist in Duluthwill also provide training to help you walk smoothly and without a limp, which may require that you use a walking aid such as a walker, crutches, or cane.
Braces that reduce the motion in the ankle can also be beneficial in reducing pain. Special braces that transfer some of the body weight to the knee can help protect the ankle. These braces are called patellar tendon bearing braces. They are quite large and bulky and may not be well tolerated by some patients.
We may recommend modifying your shoe with a rocker sole may give some relief of symptoms. The rocker sole replaces your normal sole with a rounded one, allowing your foot to roll as you move through a step. This can help take stress off the ankle as you walk.
If you don't need surgery, we may recommend that range-of-motion exercises for the ankle be started as pain eases, followed by a program of strengthening. Our program then advances to include strength and balance exercises. Your physical therapist will give you tips on keeping your symptoms controlled. Although recovery time varies among patients, as a guideline, you may progress to a home program within four to six weeks.
In cases of advanced OA where surgery is called for, patients may also see our physical therapists before surgery to discuss exercises that will be used just after surgery and to begin practicing using crutches or a walker.
Post-surgical Rehabilitation
Your ankle will be bandaged with a well-padded dressing and a splint for support after surgery. Most patients are instructed not to place weight on their foot for a period of time after surgery. After arthroscopy, this period typically lasts about one week. Although recovery time is not the same for everybody, after ankle joint replacement, most patients are usually advised to avoid placing weight on their foot for up to 12 weeks.
Physical therapy sessions, such as those provided by In Motion Therapy, may be needed after surgery for up to two months. When you visit In Motion Therapy, your first few treatments will be used to help control the pain and swelling after surgery. Treatments provided by our therapist may include electrical stimulation, ice, and soft tissue massage. We may also use hands-on joint movements and stretching to improve your range of motion and flexibility.
Our physical therapists sometimes treat patients in a pool. Exercising in a swimming pool puts less stress on the ankle joint, and the buoyancy lets you move and exercise easier. Once you've gotten your pool exercises down and the other parts of your In Motion Therapy rehab program advance, you may be instructed in an independent program.
Our physical therapist will also work with you to safely increase the amount of weight you are able to place on your foot. Our goal will be to help you walk comfortably and with a smooth walking pattern. Some of the exercises you'll do are to help strengthen and stabilize the muscles around the ankle joint. Your physical therapist will provide tips on ways to do your activities while avoiding extra strain on the ankle joint.
In Motion Therapy provides physical therapy services in Duluth.
Physician Review
Your physician may take regular X-rays to see how severely the joint is damaged. This is usually the most important test to determine how bad the OA has become. How much articular cartilage is left in the ankle joint can also be estimated with the X-rays.
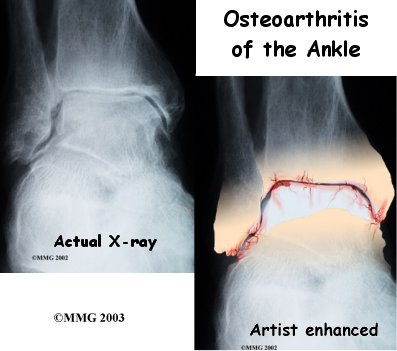
If there is any question whether the arthritis may be coming from something other than OA, blood tests may be ordered to look for systemic diseases such as rheumatoid arthritis. A needle may be inserted into the joint to remove some of the joint fluid. This fluid may be sent to a lab to look for crystals due to gouty arthritis or signs of infection.
Newer medications such as glucosamine and chondroitin sulfate are being used by orthopedic surgeons more commonly today. These medications seem to be effective in reducing the pain of OA in all joints.
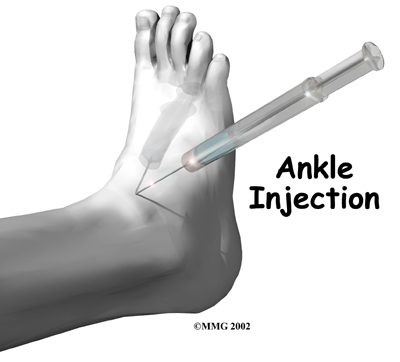
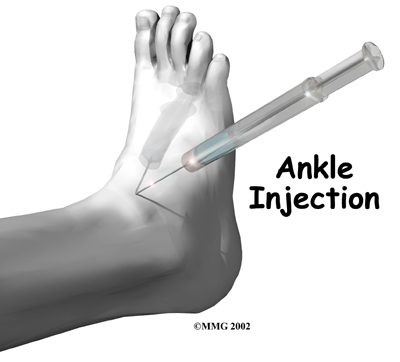 An into the joint can give temporary relief from symptoms of OA. Cortisone is a powerful anti-inflammatory medication. When injected into the joint itself, cortisone can help relieve the pain. The pain relief is temporary and usually only lasts several weeks to months. There is a small risk of infection with any injection into a joint, and cortisone injections are no exception.
An into the joint can give temporary relief from symptoms of OA. Cortisone is a powerful anti-inflammatory medication. When injected into the joint itself, cortisone can help relieve the pain. The pain relief is temporary and usually only lasts several weeks to months. There is a small risk of infection with any injection into a joint, and cortisone injections are no exception.
There are also new injectable medications that lubricate the arthritic joint. These medications have been studied mainly in the knee. It is unclear if they will help the arthritic ankle joint. These injectable medications are not usually prescribed for this condition yet.
Surgery
Eventually, it may be necessary to consider surgery for OA of the ankle. There are several different types of surgery that can be performed to help with your condition. Which procedure is recommended by your surgeon will be determined by many things. These include how much the degeneration in the ankle has progressed, how active you are, how old you are, and what other medical problems you have. Each type of procedure has risks and benefits that should be discussed with your surgeon. The choices for surgery are arthroscopic surgery to clean up the joint, fusion of the joint, or replacing the joint with an artificial ankle joint.
Arthroscopic Debridement
Sometimes when OA of the ankle occurs, loose pieces of cartilage and bone float around inside the ankle joint. These loose bodies can cause irritation in the joint, leading to inflammation. They can also get caught between the joint surfaces of the ankle. This can cause a sharp pain when it happens. The cartilage surfaces of the joint also become rough, with flaps of cartilage that peel off the surface, much like paint peeling off the ceiling. Bone spurs, or outgrowths, form around the joint and can grow larger over time. These bone spurs can rub against the soft tissues around the ankle joint when the ankle moves, again causing pain and swelling.
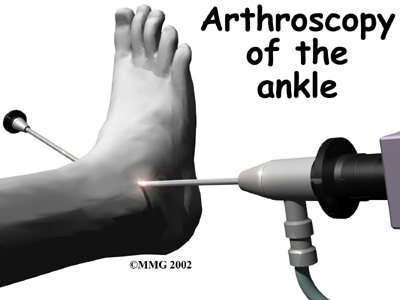 The can help the doctor remove these loose bodies and bone spurs and smooth the cartilage surfaces of the ankle joint. The arthroscope is a special TV camera that is inserted through small incisions (one-quarter of an inch) around the ankle. Small surgical tools can also be inserted through these incisions to work in the ankle joint.
The can help the doctor remove these loose bodies and bone spurs and smooth the cartilage surfaces of the ankle joint. The arthroscope is a special TV camera that is inserted through small incisions (one-quarter of an inch) around the ankle. Small surgical tools can also be inserted through these incisions to work in the ankle joint.
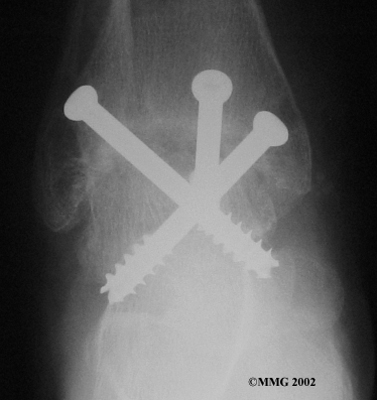
Ankle Fusion
When the ankle joint becomes so painful that it is difficult to walk, surgery may be suggested to . An ankle fusion is sometimes also called an ankle arthrodesis. In this operation, the three bones that make up the ankle joint (the talus, the tibia, and the fibula) are allowed to grow together, or fuse, into one bone. Once this is done the ankle no longer is able to move, but with a successful fusion the pain is gone. Most people with a successful fusion of the ankle are able to walk without much trouble, and in some cases it is almost impossible to tell that the ankle is stiff. But it is very difficult to run because you lose the ability to push off with the toes. The foot can't bend down.
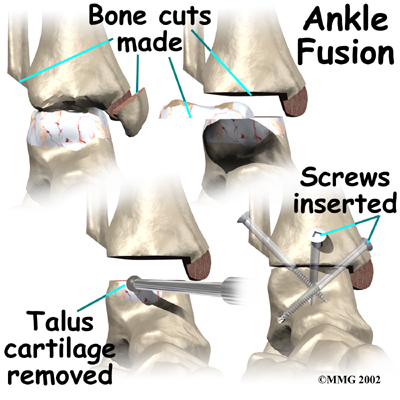
Most people will need some changes made to their shoes following an ankle fusion. Because the , it is difficult to roll over the top of the foot when you take a step. For this reason, shoes are usually fitted with a rocker sole. This allows the shoe to roll instead of the foot. A special heel is sometimes built on the shoe to absorb some of the shock.
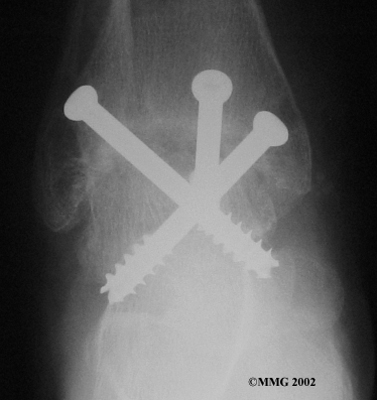
The ankle fusion is a good operation, especially for a young, active person. It is usually the preferred option for post-traumatic arthritis of the ankle. Once the ankle is successfully fused it can last a lifetime, and no other operations are expected later unless there are problems. But there are complications associated with the ankle fusion, and not all ankle fusions are successful.
Related Document: In Motion Therapy's Guide to Ankle Fusion
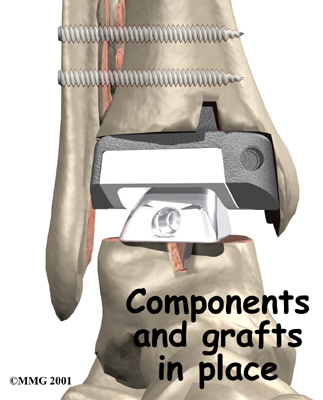
Artificial Ankle Replacement
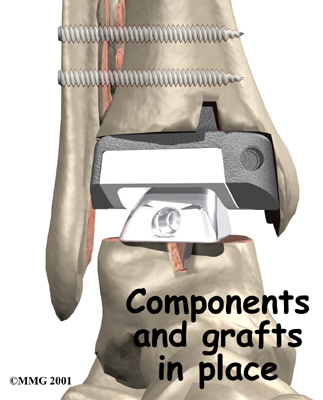 Because no one wants to lose the ability to move the ankle, much research has been done trying to perfect an . Until now, the artificial ankle has not been nearly as successful as the artificial hip or knee.
Because no one wants to lose the ability to move the ankle, much research has been done trying to perfect an . Until now, the artificial ankle has not been nearly as successful as the artificial hip or knee.
The ankle is a difficult joint to replace for many reasons. The socket (usually called the mortise) is actually made up of two bones, the tibia and the fibula. These two bones move against one another slightly when we walk. This makes it difficult to get the artificial ankle socket to stay connected to the bone.
The biggest problem with the older artificial ankle designs is that they loosened after a relatively short time and began to cause pain. When using the newer artificial ankle designs, surgeons have tried to solve this problem by actually fusing the tibia and fibula together during the operation and placing screws across the two bones. This has dramatically increased the success rate for the artificial ankle replacements done today. Many surgeons are now beginning to use the artificial ankle for post-traumatic arthritis instead of doing a fusion. Patients are able to keep the motion in the ankle and avoid some of the problems associated with the ankle fusion.
Related Document: In Motion Therapy's Guide to Artificial Ankle Replacement
Portions of this document copyright MMG, LLC.



 Injury to a joint, such as a bad sprain or fracture, can cause
Injury to a joint, such as a bad sprain or fracture, can cause 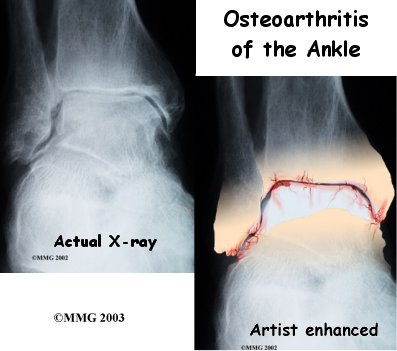
 An
An 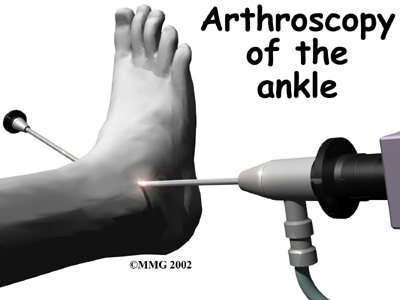 The
The 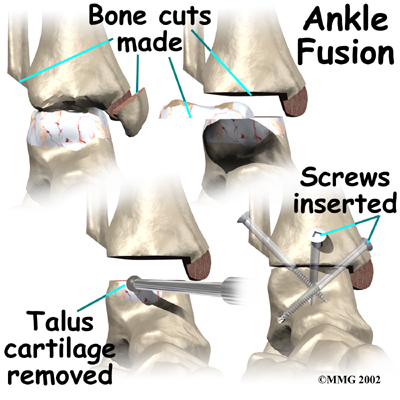
 Because no one wants to lose the ability to move the ankle, much research has been done trying to perfect an
Because no one wants to lose the ability to move the ankle, much research has been done trying to perfect an