Introduction
Physical therapy in Duluth for Shin Splints
Welcome to In Motion Therapy's patient resource about Shin Splints.
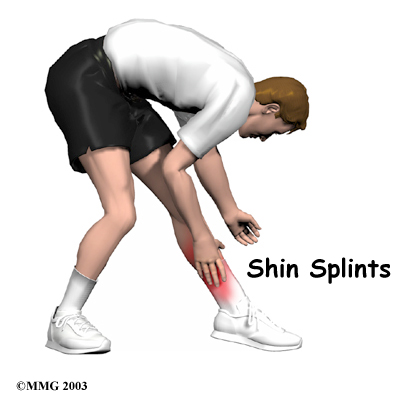
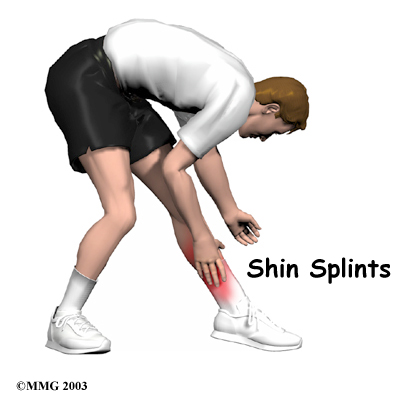
Pain along the front or inside edge of the shinbone (tibia) is commonly referred to as shin splints. The problem is common in athletes who run and jump. It is usually caused by doing too much, too quickly. The runner with this condition typically reports a recent change in training, such as increasing the usual pace, adding distance, or changing running surfaces. People who haven't run for awhile are especially prone to shin splints after they first get started, especially when they run downhill. Shin splints on the front of the tibia are called anterior shin splints. Posterior shin splints cause pain along the inside edge of the lower leg.
This guide will help you understand:
- how shin splints start
- what shin splints feel like
- how this condition is treated
Anatomy
What parts of the leg are involved?
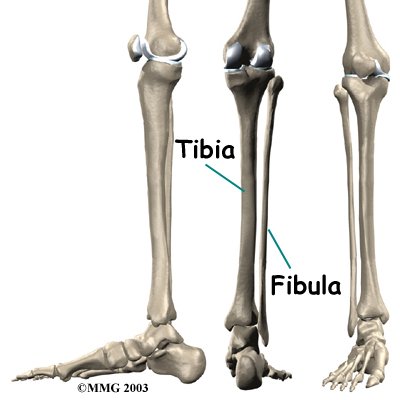
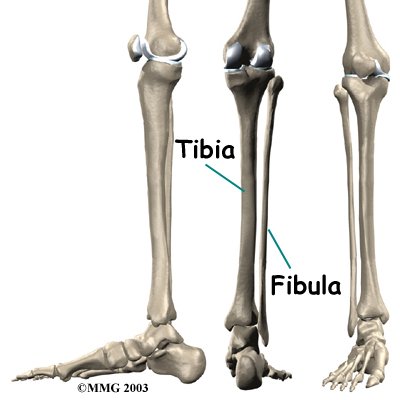
The lower leg is made up of . The shinbone is the larger of the two bones. It is called the tibia. The small, thin bone that runs alongside the tibia from the knee to the ankle is the fibula.
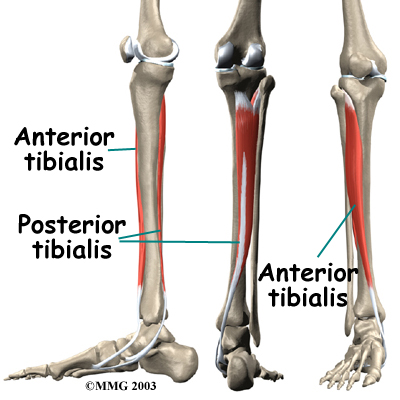
The tibia and fibula provide a connecting point for several muscles that move the foot. The main muscle that bends the foot upward connects on the front (anterior) of the tibia. It is called the anterior tibialis. The posterior tibialis, which pulls the foot down and in, attaches along the back (posterior) and inside edge of the tibia. Together, the anterior and posterior tibialis muscles are called the tibialis muscles.
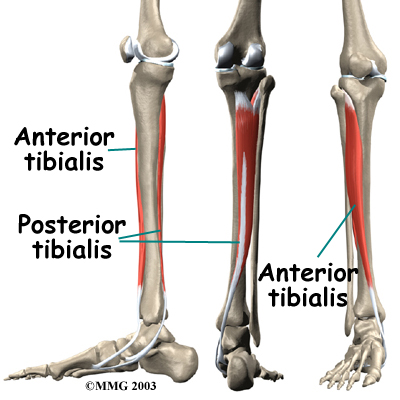
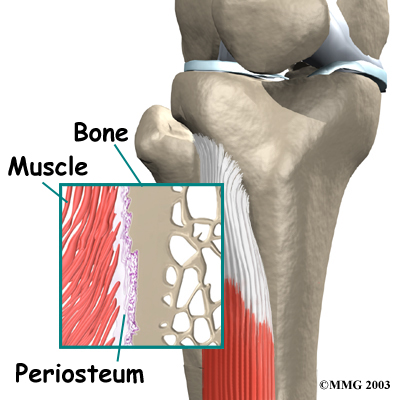
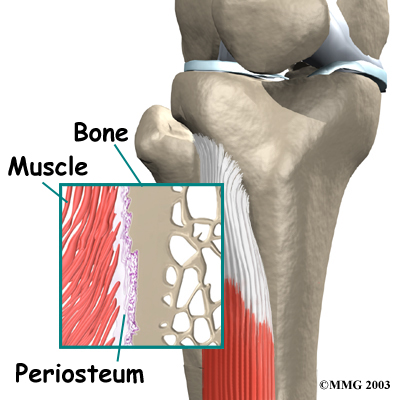
The tibialis muscles have that fasten the muscle to the bony surface of the tibia. This bony covering, or membrane, is called the periosteum (peri means around, and osteum means bone).
Related Document: In Motion Therapy's Guide to Ankle Anatomy
Causes
Why do I have shin splints?
Shin splints usually result from overuse. Repeated movements of the foot can cause damage where the tibialis muscles attach to the tibia. Soon the edge of the muscles may begin to pull away from the bone. The injured muscle and the bone covering (the periosteum) become inflamed.
Overuse commonly happens after changes in training. Increasing running speed and distance and running on hard or angled surfaces can contribute to overuse. Overuse can also occur from running in flimsy footwear or in shoes with soles that are worn out.
Anterior shin splints tend to affect people who take up a new activity, such as jogging, sprinting, or playing sports that require quick starts and stops. The unfamiliar forces place a heavy strain on the anterior tibialis muscle, causing it to become irritated and inflamed. This commonly happens when people who aren't regular runners decide to go on a long jog. The anterior tibialis muscle must work hard to control the landing of the forefoot with each stride. Running downhill puts even more demands on this muscle in order to keep the forefoot from slapping down. People who run on the balls of their feet or who run in shoes with poor shock absorption also tend to get anterior shin splints.
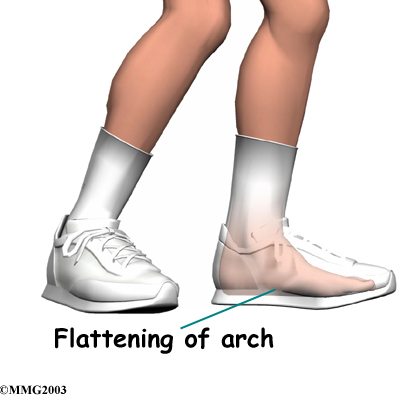
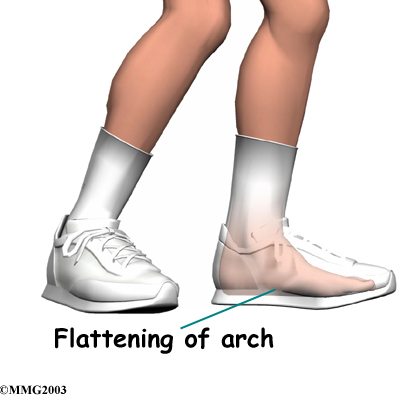 Posterior shin splints are generally caused by imbalances in the leg and foot. Muscle imbalances from tight calf muscles can cause this condition. Imbalances in foot alignment, such as having (called pronation), can also cause posterior shin splints. As the foot flattens out with each step, the posterior tibialis muscle gets stretched, causing it to repeatedly tug on its attachment to the tibia. The posterior tibialis muscle attachment eventually becomes damaged, leading to pain and inflammation along the inside edge of the lower leg.
Posterior shin splints are generally caused by imbalances in the leg and foot. Muscle imbalances from tight calf muscles can cause this condition. Imbalances in foot alignment, such as having (called pronation), can also cause posterior shin splints. As the foot flattens out with each step, the posterior tibialis muscle gets stretched, causing it to repeatedly tug on its attachment to the tibia. The posterior tibialis muscle attachment eventually becomes damaged, leading to pain and inflammation along the inside edge of the lower leg.
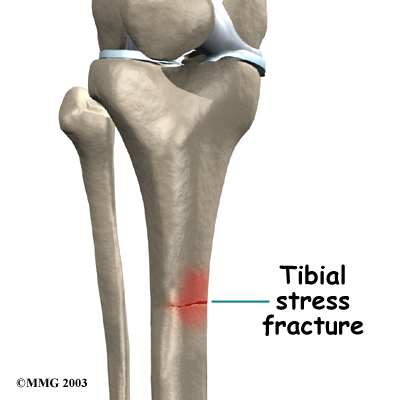
A stress fracture in the tibia is a serious problem that at first may have the same symptoms as shin splints. A stress fracture is a crack in a weakened area of bone. Continual stresses from running on hard surfaces or from heavy strain in the tibialis muscles can weaken and eventually fracture the tibia. People with shin pain who try to work through it sometimes end up developing a stress fracture in the tibia.
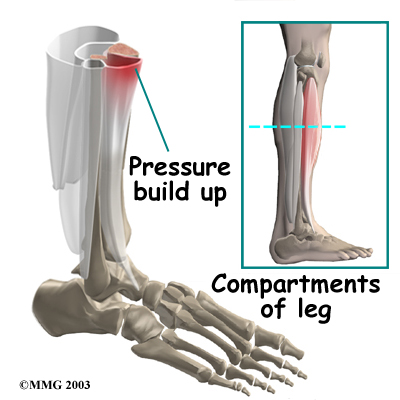
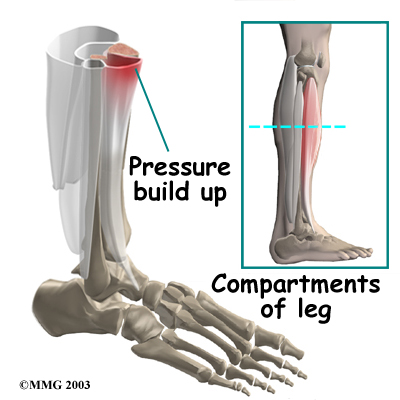
A concerning complication of shin splints is compartment syndrome. Compartment syndrome is a condition where pressure from muscle damage and swelling builds up inside a section, or compartment, within the body. There are four compartments in the lower limb. As the pressure builds in the compartment, the small blood vessels (called capillaries) that supply blood to the muscles in the compartment are squeezed shut. This happens when the pressure in the compartment is higher than the blood pressure that keeps the small blood vessels open. When the muscle loses its blood supply it begins to ache, like a muscle cramp.
If the continues to rise, it can squeeze the larger blood vessels and nerves as well. Patients may feel coldness, numbness, and swelling in the lower leg and foot. If pressure builds up and is not treated, it can cause serious tissue damage in the leg and foot.
Symptoms
What do shin splints feel like?
Dull, aching pain is felt where the involved tibialis muscle attaches to the tibia. Redness and swelling can also occur in this area. Tenderness is felt where the muscle attaches to the bone.
Anterior shin splints are usually felt on the front of the tibia, especially when using the anterior tibialis muscle to bend your foot upward.
Posterior shin splints produce symptoms along the inside edge of the lower leg. Small bumps may also be felt along the edge of the tibia in this area.
Symptoms of shin splints generally get worse with activity and ease with rest. Pain may be worse when you first get up after sleeping. The sore tibialis muscle shortens while you rest, and it stretches painfully when you put weight on your foot.
Diagnosis
The diagnosis of shin splints is usually made through physical examination and evaluation of your medical history. When you visit In Motion Therapy, our physical therapists will ask questions about your training schedule, footwear and may also want to know whether you've recently begun a new sport that requires running or jumping.
The physical examination allows us see exactly where your leg hurts. We may move your ankle in different positions and have you hold your foot against applied pressure. By stretching the tibialis muscles, and by feeling where these muscles attach on the tibia, we can begin to tell where the problem is.
A test for measuring pressure in the sore leg may be needed if you have symptoms of compartment syndrome. Our physical therapist checks pressures within the tissues of the leg, before and after exercise, to see if exercise causes the pressure readings to go up.
Some patients may be referred to a doctor for further diagnosis. Once your diagnostic examination is complete, the physical therapists at In Motion Therapy have treatment options that will help speed your recovery, so that you can more quickly return to your active lifestyle.
In Motion Therapy provides services for physical therapy in Duluth.
Our Treatment
Non-surgical Rehabilitation
The physical therapists at In Motion Therapy will help you recover through treatments designed to reduce pain and inflammation and, whenever possible, address the underlying problems causing your shin splints. The length of the physical therapy program varies for each patient, but as a guideline, you might expect to devote four to six weeks to your recovery and rehabilitation.
Reducing Inflammation
The purpose of your initial treatments at In Motion Therapy will be to reduce inflammation. Some of our patients suffering from shin splints receive iontophoresis, a technique where a mild electrical current is used to push a topical steroid medicine into the sore area. Ultrasound treatments, often used in combination with topical steroids, are also effective in halting pain and inflammation. To speed your recovery, our physical therapists may also use deep tissue massage along the junction where the sore tibialis muscle meets the tibia, followed by gentle stretching of the calf and tibialis muscles.
Our physical therapists will show you how to properly ice, rest, and if necessary, tape the injured area. Special taping techniques may be used to support the sore tissues and ease pain. However, we recommend that taping be used to help the area heal, not as a way to keep on training.
Foot Support
Your In Motion Therapy specialist will evaluate your posture and alignment to see if you have problems with pronation (arch flattening), a condition that we commonly see associated with posterior shin splints. Sometimes a small heel wedge, placed under the inside edge of the heel, is enough to ease tension on the posterior tibialis muscle. For more severe problems of pronation, we may recommend foot orthotics to support the arch and reduce stresses on the posterior tibialis muscle.
Rest and Recovery
During your recovery, stop doing the activity that caused the problem and avoid heavy training and sports activity for three to four weeks, or at least until the symptoms are under control. Rest and the application of cold packs play a key role in decreasing pain and inflammation in the early stages of treatment. Only after the pain starts to go away, should you begin to resume your normal routine.
Resuming Activity
As your pain starts to go away and you begin doing more normal activities, we will help you develop a recovery program to avoid overuse while training. This may include evaluating your running style, and suggesting tips on footwear and the use of shock-absorbing insoles. Knowing your training schedule, pace, and the surface you use can guide us in making personal recommendations as you attempt to safely resume your sport.
Post-surgical Rehabilitation
If surgery is required, your In Motion Therapy rehabilitation program will have some additional elements. You may need to use crutches for several days after surgery. Many patients are able to bear some weight on their foot within the first week. A protective dressing will cover your incisions, and the stitches are usually removed within 10 to 14 days (unless they are absorbable stitches, which will not need to be taken out).
Our physical therapists will help you recover and gradually return to your normal activity level. We may recommend the use of a stationary bike within 10 to 14 days of your surgery. If you are a runner, our physical therapy program may enable you to begin a light jogging program within six weeks and resume full activity within eight to 10 weeks, although the time required for recovery and rehabilitation varies for each individual.
In Motion Therapy provides physical therapy in Duluth.
Physician Review
Your doctor may order X-rays to make sure you don't have a stress fracture. However, recent stress injuries may not show up on X-ray for the first few weeks. In these cases, a bone scan may be ordered. A bone scan involves injecting tracers into your blood stream. The tracers then show up on special X-rays of your leg. The tracers build up in areas of extra stress to bone tissue. The extra stress can be caused by a stress fracture or an inflamed periosteum (bony covering). This condition is called periostitis.
Your doctor may also order a magnetic resonance imaging (MRI) scan. An MRI scan is a special imaging test that uses magnetic waves to create pictures of your body in slices. The MRI scan shows tendons as well as bones. It also shows abnormal swelling or scar tissue. An MRI is painless and requires no needles or injections.
Surgery
Surgery is rarely needed to correct problems of shin splints. However, shin splints that are complicated by compartment syndrome may require surgery, sometimes immediately.
 If compartment syndrome is discovered and diagnostic tests show high pressures within the tissues of the lower leg, surgery may be recommended right away. The procedure to remove the pressure is called fasciotomy. Fascia is the connective tissue around and between muscles and organs. The surgeon makes a fewon either side of the lower leg. The nearby layer of fascia within several compartments is cut and removed to reduce the pressure within the compartment. The incisions are left open at first. Tissue pressures are checked over a period of two to three days. The wounds are then closed.
If compartment syndrome is discovered and diagnostic tests show high pressures within the tissues of the lower leg, surgery may be recommended right away. The procedure to remove the pressure is called fasciotomy. Fascia is the connective tissue around and between muscles and organs. The surgeon makes a fewon either side of the lower leg. The nearby layer of fascia within several compartments is cut and removed to reduce the pressure within the compartment. The incisions are left open at first. Tissue pressures are checked over a period of two to three days. The wounds are then closed.
If the problem has been present for more than three months, the surgeon may only need to make one or two incisions to cut the layer of fascia and reduce pressure inside a single problem compartment.
Portions of this document copyright MMG, LLC.


 Posterior shin splints are generally caused by imbalances in the leg and foot. Muscle imbalances from tight calf muscles can cause this condition. Imbalances in foot alignment, such as having
Posterior shin splints are generally caused by imbalances in the leg and foot. Muscle imbalances from tight calf muscles can cause this condition. Imbalances in foot alignment, such as having 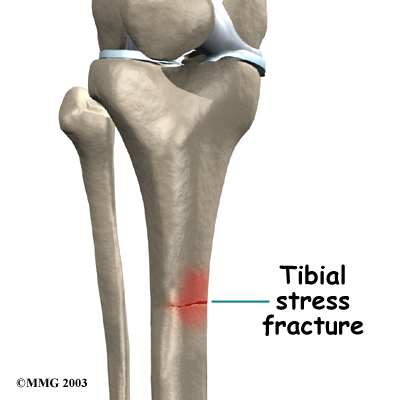
 If compartment syndrome is discovered and diagnostic tests show high pressures within the tissues of the lower leg, surgery may be recommended right away. The procedure to remove the pressure is called fasciotomy. Fascia is the connective tissue around and between muscles and organs. The surgeon makes a few
If compartment syndrome is discovered and diagnostic tests show high pressures within the tissues of the lower leg, surgery may be recommended right away. The procedure to remove the pressure is called fasciotomy. Fascia is the connective tissue around and between muscles and organs. The surgeon makes a few