Introduction
Physical therapy in Duluth for Ankle Issues
Welcome to In Motion Therapy’s guide to ankle arthroscopy.
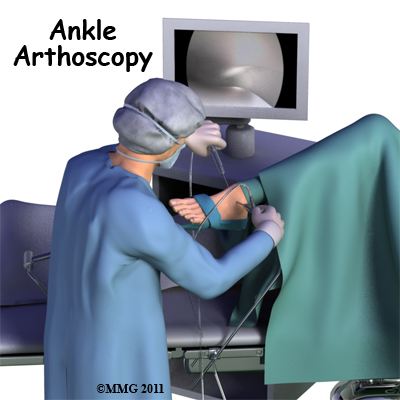
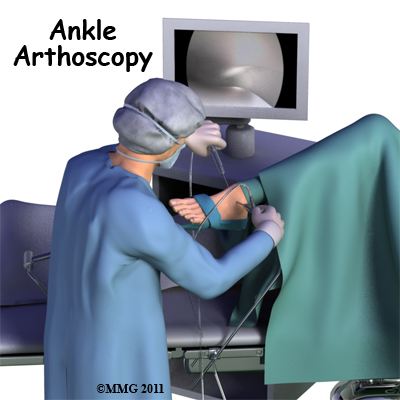
Arthroscopy is a procedure where a small video camera attached to a fiber-optic lens is inserted into the body to allow a physician or surgeon to see inside the joint without making a large incision. Arthroscopy, which is considered a minimally invasive technique, is now used to evaluate and treat orthopedic problems in many different joints of the body including the ankle.
This guide will help you understand:
- what parts of the ankle are treated during ankle arthroscopy
- what types of conditions are treated with ankle arthroscopy
- what to expect before and after ankle arthroscopy
- what In Motion Therapy’s approach to rehabilitation is
Anatomy
What parts of the ankle are involved?
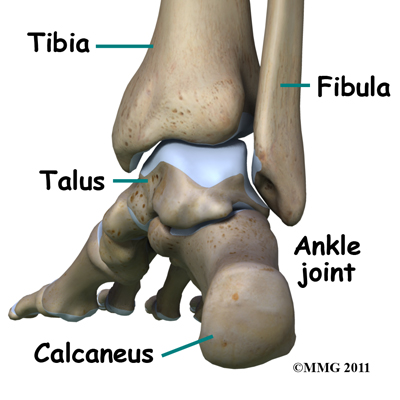
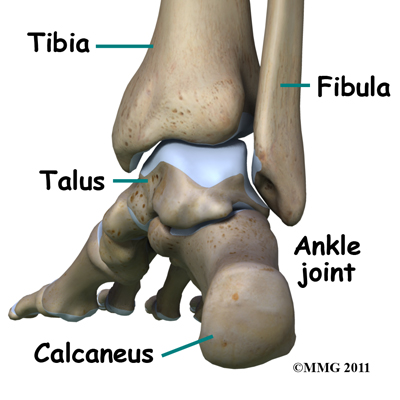
The ankle joint is formed by the connection of three bones. The top of the talus fits inside a socket that is formed by the lower end of the tibia (shinbone) and the fibula (the small bone of the lower leg). The bottom of the talus sits on the heel bone, called the calcaneus.
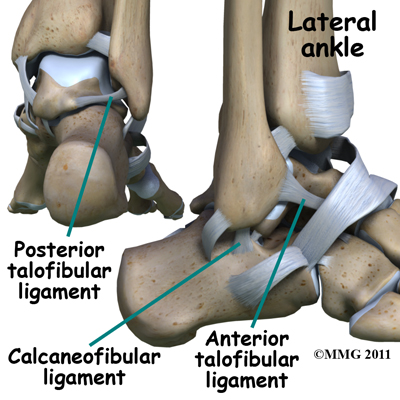
Ligaments are tough bands of tissue that connect bones together. Three ligaments make up the lateral ligament complex on the side of the ankle farthest from the other ankle. They are the anterior talofibular ligament (ATFL), the calcaneofibular ligament (CFL), and the posterior talofibular ligament (PTFL).
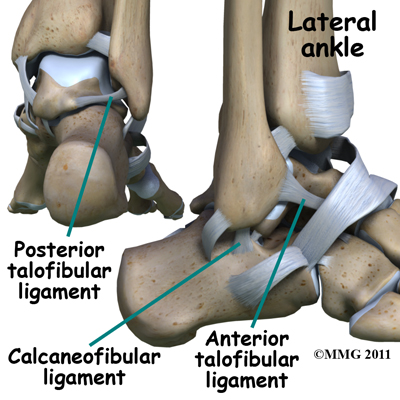
The common ankle sprain where you roll your ankle inwards (inversion ankle injury), usually involves injury to two ligaments, the ATFL and CFL. Normally, the ATFL works mostly to keep the ankle from sliding forward, and the CFL keeps the ankle from rolling inward on its side. On the opposite side of the ankle joint, closest to the other foot (the medial side), is another ligament called the deltoid ligament.
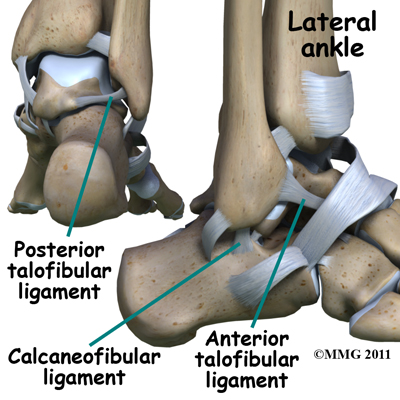
The deltoid ligament is injured much less often than the lateral ligaments of the ankle. The deltoid ligament can be torn in isolation, meaning it is the only structure injured, but this is uncommon. If it is torn in isolation it is after rolling your ankle outwards (eversion ankle injury). The deltoid ligament is most often damaged as part of a combination of injuries such as when the ankle is broken or severely sprained.
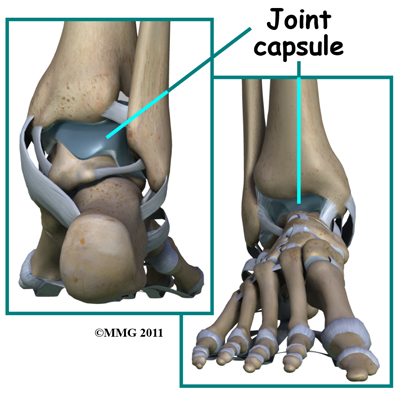
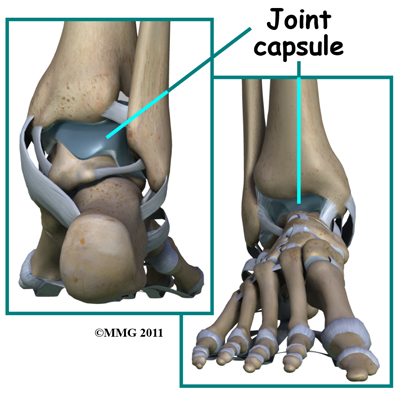
A watertight pocket called the joint capsule surrounds the ankle joint. Ligaments, connective tissue and synovial tissue form this capsule. When the joint capsule is filled with sterile saline and is distended, the surgeon can insert the arthroscope into the pocket that is formed, turn on the lights and the camera and see inside the ankle joint as if looking into an aquarium. The surgeon can see the structures that are inside the ankle joint including the joint surfaces of the distal tibia, fibula and talus and the synovial lining of the joint.
Foot Anatomy Bones & Joints
Rationale
What does my surgeon hope to accomplish?
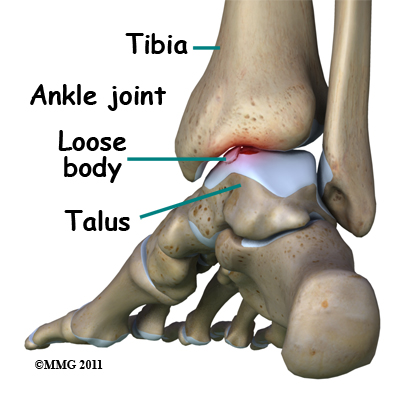
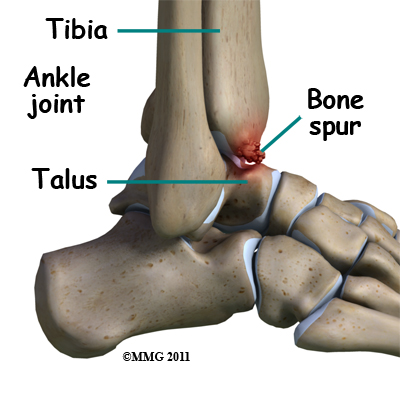
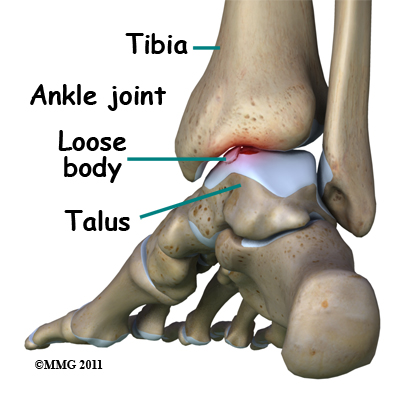
When ankle arthroscopy first became available it was used primarily to look inside the ankle joint and make a diagnosis. Today, ankle arthroscopy is used to perform a wide range of surgical procedures including confirming a diagnosis, removing loose bodies, removing bone spurs, debriding excess inflamed synovial tissue, and fixing fractures of the joint surface.
 Your surgeon's goal is to fix or improve your problem by performing a suitable surgical procedure; the arthroscope is a tool that improves the surgeon's ability to perform the appropriate procedure. The arthroscope image seen is magnified and allows the surgeon to see better and clearer as well as to perform surgery using much smaller incisions. This results in less tissue damage to normal tissue and can shorten the healing process. Remember, however, that the arthroscope is only a tool. The results that you can expect from an ankle arthroscopy depend on what is wrong with your ankle, what can be done inside your ankle to improve the problem, and your effort at physical therapy after the surgery.
Your surgeon's goal is to fix or improve your problem by performing a suitable surgical procedure; the arthroscope is a tool that improves the surgeon's ability to perform the appropriate procedure. The arthroscope image seen is magnified and allows the surgeon to see better and clearer as well as to perform surgery using much smaller incisions. This results in less tissue damage to normal tissue and can shorten the healing process. Remember, however, that the arthroscope is only a tool. The results that you can expect from an ankle arthroscopy depend on what is wrong with your ankle, what can be done inside your ankle to improve the problem, and your effort at physical therapy after the surgery.
Preparations
What do I need to know before surgery?
 You and your surgeon should make the decision to proceed with surgery as a treatment option together. You need to understand as much about the procedure as possible. If you have concerns or questions, be sure and speak to your surgeon.
You and your surgeon should make the decision to proceed with surgery as a treatment option together. You need to understand as much about the procedure as possible. If you have concerns or questions, be sure and speak to your surgeon.
Once you decide on surgery, you need to take several steps. Firstly your surgeon may suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
You will also need to spend time with a physical therapist at In Motion Therapy who will be managing your rehabilitation after surgery. This allows you to get a head start on your recovery. One purpose of this preoperative visit is to record a baseline of information. The therapist will check your current pain levels, ask you about your ability to do daily activities and discuss which activities aggravate or ease your current ankle pain. They will also assess the range of motion, strength, endurance, and proprioception in both ankles (proprioception is the ability to know where your body is without looking at it). Any muscle imbalances that you may have developed due to your current injury will also be investigated. This will require them to look at other areas in addition to your ankle, such as your knee or hip. They will also want to watch you walk and move to get an idea of your pre-operative status and your biomechanical alignment.
A second purpose of the preoperative physical therapy visit is to prepare you for the rehabilitation that you will do after your surgery. Your therapist will teach you how to walk safely using crutches or a walker, including showing you how to do stairs. They will also teach you some of the exercises you will use during your recovery and will encourage you to begin the exercises even before surgery to make the ankle as strong as possible prior beforehand.
On the day of your surgery, you will probably be admitted for surgery early in the morning. You shouldn't eat or drink anything after midnight the night before.
Surgical Procedure
What happens during ankle arthroscopy?
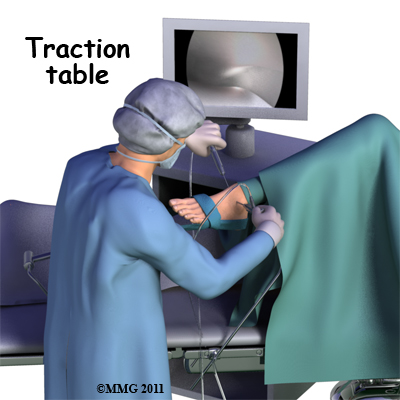
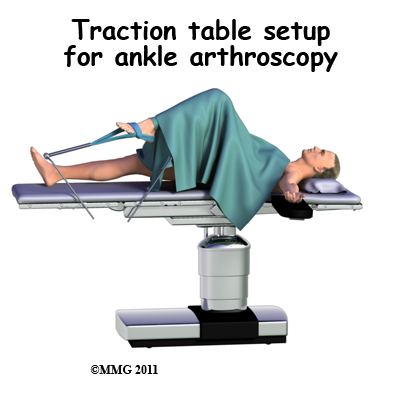 Before surgery you will be placed under either a general anesthesia or a type of spinal anesthesia. Sterile drapes are placed to create a sterile environment for your surgeon to work. There is a great deal of equipment that surrounds the operating table including the TV screens, cameras, light sources and surgical instruments. Your surgeon will apply traction to your ankle joint. The ankle joint is very tight with little space between the tibia and the talus so by applying traction, your surgeon is able to increase this space and allow the arthroscope to be inserted into that space. The end of the arthroscope will be moved about in this space to look throughout the joint.
Before surgery you will be placed under either a general anesthesia or a type of spinal anesthesia. Sterile drapes are placed to create a sterile environment for your surgeon to work. There is a great deal of equipment that surrounds the operating table including the TV screens, cameras, light sources and surgical instruments. Your surgeon will apply traction to your ankle joint. The ankle joint is very tight with little space between the tibia and the talus so by applying traction, your surgeon is able to increase this space and allow the arthroscope to be inserted into that space. The end of the arthroscope will be moved about in this space to look throughout the joint.
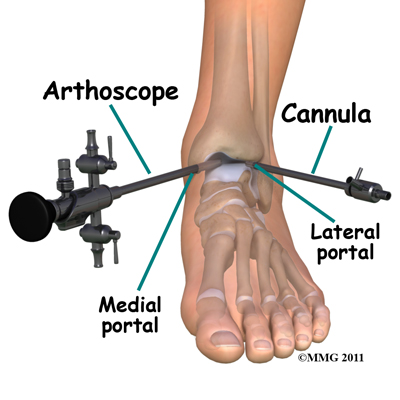
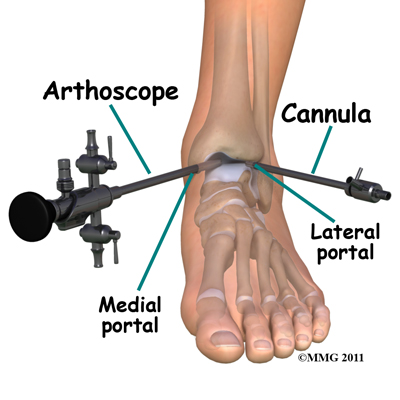
Your surgeon begins the operation by making two or three small openings into the ankle, called portals. These portals are where the arthroscope and surgical instruments are placed inside the ankle. Care is taken to protect the nearby nerves and blood vessels. A small metal or plastic tube (cannula) is placed through one of the portals to inflate the ankle with sterile saline.
The arthroscope, as explained above, is a small fiber-optic tube about 1/4 inch in diameter (slightly smaller than a pencil) and about 7 inches in length. The fiber optics inside the metal tube of the arthroscope allows a bright light and TV camera to be connected to the outer end of the arthroscope. The light shines through the fiber optic tube and into the ankle joint. A TV camera is attached to the lens on the outer end of the arthroscope. The TV camera projects the image from inside the ankle joint on a TV screen next to the surgeon. The surgeon actually watches the TV screen (not the ankle) while moving the arthroscope to different places inside the ankle joint.
 Over the years since the invention of the arthroscope, many very specialized instruments have been developed to perform different types of surgery using the arthroscope in order to see what is going on while the instruments are being used. Today, many surgical procedures that once required large incisions for the surgeon to see and fix the problem can be done via arthroscopy with much smaller incisions. For example, simple removal of a loose body in the ankle can be done using two or three small ¼ inch incisions. More extensive surgical procedures may require larger incisions. Your surgeon may decide during the procedure that the problem requires a more traditional open type operation that uses a standard surgical incision. If your surgeon has discussed this possibility with you (before the operation) he or she may create the incision immediately and complete the needed procedure via the open incision. If this has not been discussed with you beforehand, the arthroscopic procedure will be concluded and an open incision operation planned at a later date. Your surgeon will discuss with you the details of what was found at the time of the arthroscopy and what more needs to be done in the later operation.
Over the years since the invention of the arthroscope, many very specialized instruments have been developed to perform different types of surgery using the arthroscope in order to see what is going on while the instruments are being used. Today, many surgical procedures that once required large incisions for the surgeon to see and fix the problem can be done via arthroscopy with much smaller incisions. For example, simple removal of a loose body in the ankle can be done using two or three small ¼ inch incisions. More extensive surgical procedures may require larger incisions. Your surgeon may decide during the procedure that the problem requires a more traditional open type operation that uses a standard surgical incision. If your surgeon has discussed this possibility with you (before the operation) he or she may create the incision immediately and complete the needed procedure via the open incision. If this has not been discussed with you beforehand, the arthroscopic procedure will be concluded and an open incision operation planned at a later date. Your surgeon will discuss with you the details of what was found at the time of the arthroscopy and what more needs to be done in the later operation.
Once the surgical procedure is complete, the arthroscopic portals and surgical incisions will be closed with sutures, surgical staples, or surgical strips. You may be placed in a large compressive bandage and a splint that goes from the knee to the toes. The splint and bandage are used to immobilize and protect the ankle. If your surgeon feels that you do not need a bulky bandage and splint, you may be placed in thin compression stockings. A compressive bandage (or stocking) reduces swelling and helps to prevent blood clots in the leg. Once the bandage has been put on you will be taken to the recovery room.
Ankle arthroscopy is usually done on an outpatient basis meaning that patients go home the same day as the surgery. More complex reconstructions that require larger incisions and surgery that alters bone may require a short stay in the hospital to control pain more aggressively and monitor the situation carefully. You may also begin physical therapy while in the hospital.
Crutches are commonly used after ankle arthroscopy. They may only be needed for one to two days after simple procedures. A physical therapist will visit you in the hospital to teach you how to safely use crutches both on level ground and on stairs. If it is too difficult for you to use crutches then they will teach you how to walk on level ground with a walker instead. You will need to follow your surgeon's instructions about how much weight to place on your foot while standing or walking. How much weight your surgeon would like you to put on your surgical side depends on what your surgeon has done inside your ankle. Every surgery is different. Crutches may only be needed for one to two days after simple procedures, but should always be used until your surgeon says you can fully weight bear, and until you can walk virtually without a limp. Even one crutch, used on the opposite side to your injury, can be used to provide some support and allow you to avoid walking with a compensatory gait post-surgically.
It is important to avoid doing too much, too quickly. You will be instructed to use a cold pack on the ankle and to keep your leg elevated and supported while sitting or laying both in the hospital and when you go home. Your physical therapist will instruct you to perform toe-wiggling exercises in order to assist with moving swelling from your lower leg and to prevent the blood in your legs from clotting. Depending on what was done in your surgery and if your surgeon allows it your physical therapist may encourage you to perform simple ankle circle exercises as well as ankle pumping exercises within your pain tolerance level. These exercises assist in both initiating range of motion, and in moving the swelling from your lower leg.
Complications
What can go wrong?
As with all major surgical procedures, complications can occur during ankle arthroscopy. This document doesn't provide a complete list of the possible complications, but it does highlight some of the most common problems, which are:
- anesthesia complications
- thrombophlebitis
- infection
- equipment failure
- slow recovery
Anesthesia Complications
Most surgical procedures require some type of anesthesia to be used. A very small number of patients have problems with anesthesia. These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthetic state itself. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
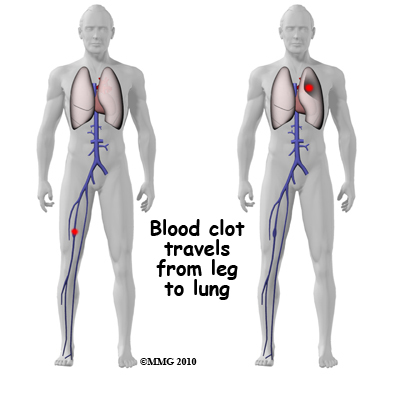 Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when blood clots form in the large veins of the leg. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism (pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective method is to get you moving as soon as possible after the surgery. Two other commonly used preventative measures include:
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when blood clots form in the large veins of the leg. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism (pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective method is to get you moving as soon as possible after the surgery. Two other commonly used preventative measures include:
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Following ankle arthroscopy, it is possible that a postoperative infection may occur. This is very uncommon and happens in less than 1% of cases. You may experience increased pain, swelling, fever and redness or drainage from the incisions. You should alert your surgeon if you think you are developing an infection.
Infections are of two types: superficial or deep. A superficial infection may occur in the skin around the incisions or portals. A superficial infection does not extend into the joint and can usually be treated with antibiotics alone. If the ankle joint itself becomes infected, this is a serious complication and will require antibiotics and possibly another surgical procedure to drain the infection.
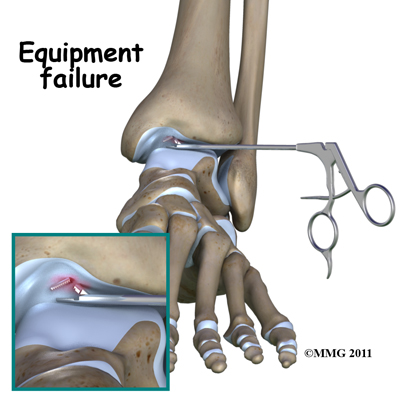
Equipment Failure
Many of the instruments used by the surgeon to perform ankle arthroscopy are small and fragile. These instruments can break resulting in a piece of the instrument floating inside of the joint. The broken piece is usually easily located and removed, but this may cause the operation to last longer than planned. There is usually no damage to the joint due to the breakage.
Different types of surgical devices (screws, pins and suture anchors) are used to hold tissues in place during and after arthroscopy. These pieces of equipment can also cause problems. If one of these devices breaks, the free-floating piece may hurt other parts inside the joint, particularly the articular cartilage. Another problem may be that the end of the device may poke too far through tissue and the point may rub and irritate other tissues. If any of these things occur a second surgery may be needed to remove the device or fix the problem.
Slow Recovery
 Not everyone gets quickly back to routine activities after ankle arthroscopy. Because the arthroscope allows surgeons to use smaller incisions than in the past, many patients mistakenly believe that less surgery was necessary. This is not always true. The arthroscope allows surgeons to do a great deal of reconstructive surgery inside the ankle joint without making large incisions. How fast you recover from ankle arthroscopy depends on what type of surgery was done inside your ankle. Simple problems that require simple procedures using the arthroscope generally get better faster. Patients with extensive damage to the articular cartilage in the ankle joint tend to require more complex and extensive surgical procedures. These more extensive reconstructions take longer to heal and have a slower recovery. You should discuss the recovery process with your surgeon and make sure that you have realistic expectations of what to expect following arthroscopic ankle surgery. The effort you put into your rehabilitation program after surgery can also affect how quickly you recover, however, this still depends on what procedure was done inside of your ankle.
Not everyone gets quickly back to routine activities after ankle arthroscopy. Because the arthroscope allows surgeons to use smaller incisions than in the past, many patients mistakenly believe that less surgery was necessary. This is not always true. The arthroscope allows surgeons to do a great deal of reconstructive surgery inside the ankle joint without making large incisions. How fast you recover from ankle arthroscopy depends on what type of surgery was done inside your ankle. Simple problems that require simple procedures using the arthroscope generally get better faster. Patients with extensive damage to the articular cartilage in the ankle joint tend to require more complex and extensive surgical procedures. These more extensive reconstructions take longer to heal and have a slower recovery. You should discuss the recovery process with your surgeon and make sure that you have realistic expectations of what to expect following arthroscopic ankle surgery. The effort you put into your rehabilitation program after surgery can also affect how quickly you recover, however, this still depends on what procedure was done inside of your ankle.
Rehabilitation
After ankle arthroscopy rehabilitation at In Motion Therapy should begin as soon as possible. There are a few cases where your surgeon may delay a start in your therapy because they want the tissues to heal with rest before any further stress is placed on the ankle. Often therapy begins, however, before you are even allowed to fully weight bear. In other cases, rehabilitation will not be recommended until full or nearly full weight bearing begins. Each surgeon will set his or her own specific restrictions based on what was done during the surgical procedure, their personal experience, and whether your tissues are healing as expected. Generally speaking, the more complex the surgery the more involved and prolonged your rehabilitation program will be.
If you are still using crutches by the time we first see you at In Motion Therapy, your physical therapist will ensure you are using the crutches safely, properly, and confidently and that you are abiding by your weight bearing restrictions. They will also ensure that you can safely use your crutches on stairs. If you are no longer using crutches, or once you no longer need them, your physical therapist will focus on normal gait re-education so you are putting only the necessary forces through your surgical ankle with each step, and are not compensating in any way. As mentioned above, until you are able to walk without a significant limp, we recommend that you continue to use your crutches, or at least one crutch or a cane/walking stick. Improper gait can lead to a host of other pains in the knee, hip and back so it is prudent to use a walking aid until near normal walking can be achieved. Your physical therapist at In Motion Therapy will monitor how well you are walking and advise you regarding the appropriate time for you to be ambulating without any walking aid at all.

During your first few appointments at In Motion Therapy your physical therapist will focus on relieving the pain and inflammation from the surgical procedure itself. We may use modalities such as ice, heat, ultrasound, or electrical current to assist with decreasing any pain or swelling you have around the surgical site or anywhere up the extremity. In addition, your physical therapist may massage your leg and ankle to improve circulation and help decrease your pain.
The next part of our treatment will focus on regaining the range of motion in your ankle. Your physical therapist at In Motion Therapy will prescribe a series of stretching exercises that you will practice in the clinic and also learn to do as part of a home exercise program. The majority of your ankle range of motion generally comes back very quickly after an arthroscopic surgery, but it still depends on what your surgeon has done inside your joint. You may experience a small amount of discomfort at the end ranges of ankle motion initially, but it is still important to do the range of motion exercises that your therapist prescribes as moving the joint also helps to move the swelling, get fresh blood to the healing area, and provide nutrition to the surface of the joint. Only mild discomfort, however, is permissible. Any sharp or moderate discomfort should be heeded. Exercises such as ankle circles and ankle pumping will begin to assist your range of motion. Other stretching exercises which address your ankle’s ability to bend up and point downwards as well as move the ankle inwards and outwards will also be prescribed along with stretches for your calf. An exercise bike at this stage is very useful to assist in gaining back the initial stages of ankle range of motion. By adjusting the bike seat to a higher than normal level, and perhaps even tilting your hips or adjusting your foot position as you rotate the pedal around, you should be able to get the pedal around in a full rotation, which will encourage ankle bending. Even if you are unable to fully rotate the pedals, stationary cycling where you rotate back and forth within your limits is still encouraged at this stage as the back and forth motion forces fluid through the joint and greatly assists the healing process in addition to encouraging improved range of motion. Once you can easily rotate the pedals around and you have the seat at your normal or slightly lower position, the stationary cycle is no longer useful for improving ankle range of motion. At this stage your therapist will prescribe more advanced ankle range of motion exercises. Using the stationary cycle to maintain or improve your cardiovascular fitness, however, is still encouraged and highly recommended to maintain the rest of your body’s fitness while your ankle is healing.
Maintaining overall fitness can actually begin very early post-surgically. You can use an upper body bike if you are non-weight bearing or don’t have the range of motion to use a stationary cycle, or you may be allowed to do non-weight bearing cardiovascular exercise in a pool. Weights for the upper extremities and other leg are also strongly encouraged as you recover from your ankle surgery. Your physical therapist at In Motion Therapy can provide a program for you to maintain your general fitness while you recover from your surgery.
In order to gain maximal range of motion and to do it as quickly as possible your physical therapist will mobilize your ankle joint. This hands-on technique encourages the ankle to move gradually into its normal range of motion. Mobilizations by your therapist may be combined with stretching of the calf muscles or bending of the knee. These combined techniques help to gain maximum end range of motion of the ankle as well as to encourage the ankle motion to return in a more functional manner, which means that the motions or exercises more closely mimic everyday activities such as walking or stair climbing.
As soon as possible your therapist will prescribe strengthening exercises for your ankle. These exercises will focus on the muscles around your ankle but will also include some exercises for your hip and knee area as these areas play a large supporting role for your ankle. Exercise band is often used to add extra resistance to the muscles supporting the ankle. Your body weight will also be used as resistance for some of the ankle strengthening exercises such as calf raises. Weights may also be used to add even further weight to the ankle as it tolerates it. Exercises that involve the entire lower limb like squats will be prescribed. Given that these exercises are done in a weight bearing position they are more functional for everyday activities such as walking or doing stairs. Exercises such as squats also force the ankle to work together with the knee and hip in order to maintain proper lower extremity alignment. Other non-weight bearing exercises in sitting or lying, however, can also be important and may be prescribed. Non-weight bearing exercises can allow you to target specific muscles around the ankle, as well as to target other muscles that help support the ankle such as the gluteal muscles of the hip. If you have access to a pool, your therapist may suggest you go to the pool to do your specific ankle exercises. The buoyancy of the water along with the water’s warmth can assist greatly in providing comfort to the ankle joint and often allows you to exercise more easily with less discomfort.
As a result of any injury, the receptors in your joints and ligaments that assist with balance and proprioception (the ability to know where your body is without looking at it) decline in function. A period of immobility and reduced weight bearing will add to this decline. Due to the invasive nature of surgery it can be considered a controlled ‘injury’ to the joint, and thereby can cause a decline in these receptors. If your balance and proprioception has declined, your joint and your limb as a whole will not be as efficient in it’s functioning and the decline may contribute to further injury in the future. The ankle joint, being the bottom of the anatomical chain, has many receptors that assist with proprioception. These proprioceptive receptors are extremely important in the recovery of your ankle from surgery, and also important in preventing another injury. Your physical therapist at In Motion Therapy will prescribe exercises for you to regain your balance and ankle proprioception. These exercises might include activities such as standing on one foot or balancing on an unstable surface such as a wobbly board or a soft plastic disc. Standing on your tippy toes on your surgical side is another proprioceptive exercise. Closing your eyes during these exercises challenges the receptors even further. Advanced exercises will include agility type activities such as hopping, moving side to side, or turning directions as you jump.
To assist with your rehabilitation your therapist may tape your ankle. Taping the ankle may help you do exercises and activities with less pain and assist in supporting your ankle until the muscles are strong enough to do this themselves. Your physical therapist may even teach you how to tape your own ankle. You may not need to use tape for a long period, although some patients like to use it long term to provide support to the ankle. Taping over a longer time frame often causes irritation to the skin and can be cumbersome, therefore if the taping helps, a brace, which performs a similar function, may be suggested. An initial trial of taping is often an easy and cost-effective way to determine if a brace will in fact decrease your pain and assist you with support before actually investing in a brace.
Several ankle braces are available on the market and may be useful for you to use both as your ankle recovers from the surgery and also as you return to more advanced activities such as the sports you enjoy participating in. Your physical therapist can educate you on whether a brace would be useful for you as well as the most appropriate one for your ankle.
As your range of motion, strength, and proprioception improve, your therapist will advance your exercises to ensure your rehabilitation is progressing as quickly as your body allows. As soon as it is safe to do so, your therapist will add more aggressive rehabilitation exercises such as jumping from a height, repetitive hopping, running, and exercises that mimic the sports or recreational activities that you participate in. During all of your exercises you therapist will pay particular attention to your technique to ensure that you are not using any compensatory patterns or are developing bad habits in regards to how you use your ankle and entire lower extremity. If you do not pay close attention to how you use your joint and limb post-surgically poor patterns that have developed over years of use often continue to occur once the source of your pain has been dealt with by the arthroscopic surgery. Your physical therapist at In Motion Therapy will be crucial to providing you with feedback regarding correcting these patterns and developing new, efficient patterns during your daily activities.
Today, the arthroscope is used to perform quite complicated and major reconstructive surgery using very small incisions. Remember, however, that just because you have small incisions on the outside, there may be a great deal of healing tissue on the inside of the ankle joint. If you have had major reconstructive surgery, you should expect full recovery to take several months.
When you are well under way, regular visits to In Motion Therapy will end. Your therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.
Generally rehabilitation after arthroscopic ankle surgery proceeds very smoothly with the physical therapy we provide at In Motion Therapy. If for some reason, however, your pain continues longer than it should or therapy is not progressing as your physical therapist would expect, we will ask you to follow-up with your surgeon to confirm that the ankle is tolerating the rehabilitation well and to ensure that there are no complications that may be impeding your recovery.
Portions of this document copyright MMG, LLC.
In Motion Therapy provides services for physical therapy in Duluth.


 Your surgeon's goal is to fix or improve your problem by performing a suitable surgical procedure; the arthroscope is a tool that improves the surgeon's ability to perform the appropriate procedure. The arthroscope image seen is magnified and allows the surgeon to see better and clearer as well as to perform surgery using much smaller incisions. This results in less tissue damage to normal tissue and can shorten the healing process. Remember, however, that the arthroscope is only a tool. The results that you can expect from an ankle arthroscopy depend on what is wrong with your ankle, what can be done inside your ankle to improve the problem, and your effort at physical therapy after the surgery.
Your surgeon's goal is to fix or improve your problem by performing a suitable surgical procedure; the arthroscope is a tool that improves the surgeon's ability to perform the appropriate procedure. The arthroscope image seen is magnified and allows the surgeon to see better and clearer as well as to perform surgery using much smaller incisions. This results in less tissue damage to normal tissue and can shorten the healing process. Remember, however, that the arthroscope is only a tool. The results that you can expect from an ankle arthroscopy depend on what is wrong with your ankle, what can be done inside your ankle to improve the problem, and your effort at physical therapy after the surgery.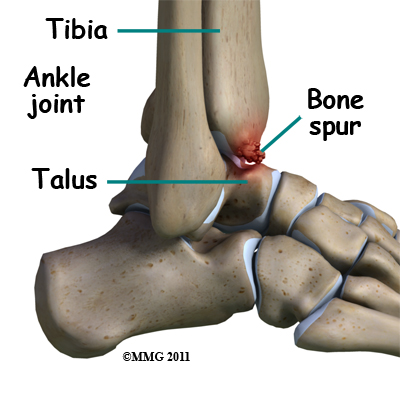 You and your surgeon should make the decision to proceed with surgery as a treatment option together. You need to understand as much about the procedure as possible. If you have concerns or questions, be sure and speak to your surgeon.
You and your surgeon should make the decision to proceed with surgery as a treatment option together. You need to understand as much about the procedure as possible. If you have concerns or questions, be sure and speak to your surgeon.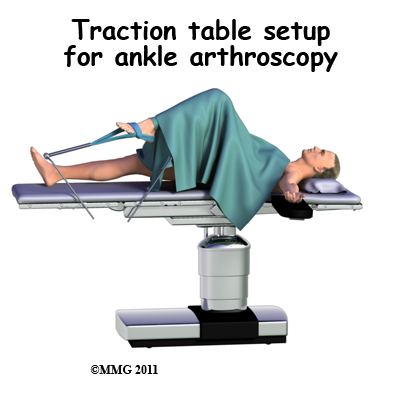 Before surgery you will be placed under either a general anesthesia or a type of spinal anesthesia. Sterile drapes are placed to create a sterile environment for your surgeon to work. There is a great deal of equipment that surrounds the operating table including the TV screens, cameras, light sources and surgical instruments. Your surgeon will apply traction to your ankle joint. The ankle joint is very tight with little space between the tibia and the talus so by applying traction, your surgeon is able to increase this space and allow the arthroscope to be inserted into that space. The end of the arthroscope will be moved about in this space to look throughout the joint.
Before surgery you will be placed under either a general anesthesia or a type of spinal anesthesia. Sterile drapes are placed to create a sterile environment for your surgeon to work. There is a great deal of equipment that surrounds the operating table including the TV screens, cameras, light sources and surgical instruments. Your surgeon will apply traction to your ankle joint. The ankle joint is very tight with little space between the tibia and the talus so by applying traction, your surgeon is able to increase this space and allow the arthroscope to be inserted into that space. The end of the arthroscope will be moved about in this space to look throughout the joint. 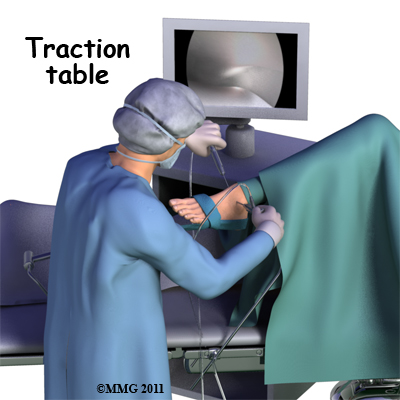
 Over the years since the invention of the arthroscope, many very specialized instruments have been developed to perform different types of surgery using the arthroscope in order to see what is going on while the instruments are being used. Today, many surgical procedures that once required large incisions for the surgeon to see and fix the problem can be done via arthroscopy with much smaller incisions. For example, simple removal of a loose body in the ankle can be done using two or three small ¼ inch incisions. More extensive surgical procedures may require larger incisions. Your surgeon may decide during the procedure that the problem requires a more traditional open type operation that uses a standard surgical incision. If your surgeon has discussed this possibility with you (before the operation) he or she may create the incision immediately and complete the needed procedure via the open incision. If this has not been discussed with you beforehand, the arthroscopic procedure will be concluded and an open incision operation planned at a later date. Your surgeon will discuss with you the details of what was found at the time of the arthroscopy and what more needs to be done in the later operation.
Over the years since the invention of the arthroscope, many very specialized instruments have been developed to perform different types of surgery using the arthroscope in order to see what is going on while the instruments are being used. Today, many surgical procedures that once required large incisions for the surgeon to see and fix the problem can be done via arthroscopy with much smaller incisions. For example, simple removal of a loose body in the ankle can be done using two or three small ¼ inch incisions. More extensive surgical procedures may require larger incisions. Your surgeon may decide during the procedure that the problem requires a more traditional open type operation that uses a standard surgical incision. If your surgeon has discussed this possibility with you (before the operation) he or she may create the incision immediately and complete the needed procedure via the open incision. If this has not been discussed with you beforehand, the arthroscopic procedure will be concluded and an open incision operation planned at a later date. Your surgeon will discuss with you the details of what was found at the time of the arthroscopy and what more needs to be done in the later operation.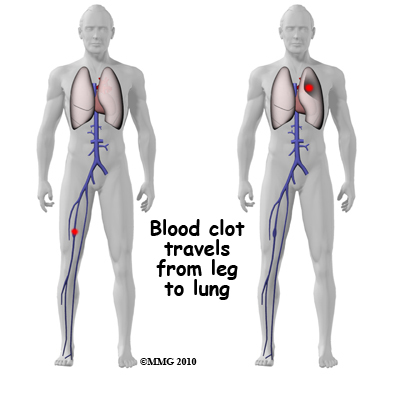 Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when blood clots form in the large veins of the leg. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism (pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective method is to get you moving as soon as possible after the surgery. Two other commonly used preventative measures include:
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when blood clots form in the large veins of the leg. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism (pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective method is to get you moving as soon as possible after the surgery. Two other commonly used preventative measures include: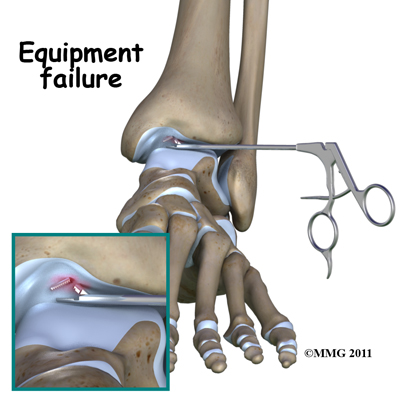 Not everyone gets quickly back to routine activities after ankle arthroscopy. Because the arthroscope allows surgeons to use smaller incisions than in the past, many patients mistakenly believe that less surgery was necessary. This is not always true. The arthroscope allows surgeons to do a great deal of reconstructive surgery inside the ankle joint without making large incisions. How fast you recover from ankle arthroscopy depends on what type of surgery was done inside your ankle. Simple problems that require simple procedures using the arthroscope generally get better faster. Patients with extensive damage to the articular cartilage in the ankle joint tend to require more complex and extensive surgical procedures. These more extensive reconstructions take longer to heal and have a slower recovery. You should discuss the recovery process with your surgeon and make sure that you have realistic expectations of what to expect following arthroscopic ankle surgery. The effort you put into your rehabilitation program after surgery can also affect how quickly you recover, however, this still depends on what procedure was done inside of your ankle.
Not everyone gets quickly back to routine activities after ankle arthroscopy. Because the arthroscope allows surgeons to use smaller incisions than in the past, many patients mistakenly believe that less surgery was necessary. This is not always true. The arthroscope allows surgeons to do a great deal of reconstructive surgery inside the ankle joint without making large incisions. How fast you recover from ankle arthroscopy depends on what type of surgery was done inside your ankle. Simple problems that require simple procedures using the arthroscope generally get better faster. Patients with extensive damage to the articular cartilage in the ankle joint tend to require more complex and extensive surgical procedures. These more extensive reconstructions take longer to heal and have a slower recovery. You should discuss the recovery process with your surgeon and make sure that you have realistic expectations of what to expect following arthroscopic ankle surgery. The effort you put into your rehabilitation program after surgery can also affect how quickly you recover, however, this still depends on what procedure was done inside of your ankle.