Introduction
Physical therapy in Duluth for Elbow
Welcome to In Motion Therapy's patient resource about Distal Biceps Rupture.
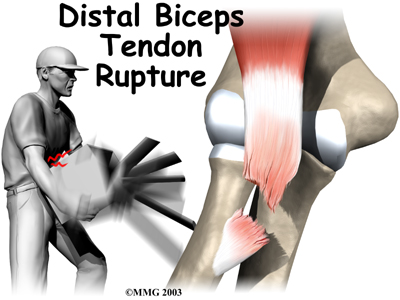
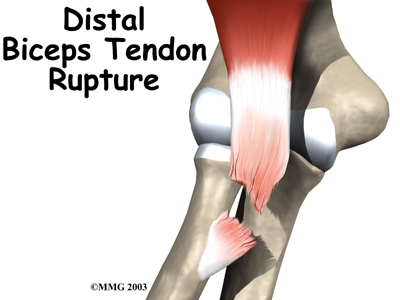
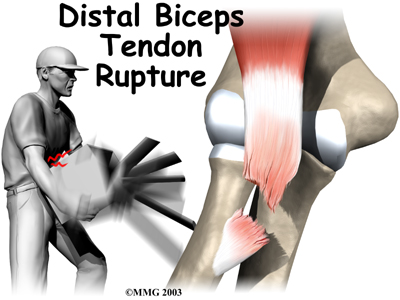
A distal biceps rupture occurs when the tendon attaching the biceps muscle to the elbow is torn from the bone. This injury occurs mainly in middle-aged men during heavy work or lifting. A distal biceps rupture is rare compared to ruptures where the top of the biceps connects at the shoulder. Distal biceps ruptures make up only three percent of all biceps tendon ruptures.
This article will help you understand:
- what parts of the elbow are affected
- the causes of distal biceps rupture
- ways to treat this problem
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Elbow Pain|limit:15|heading:Hear from some of our patients who we treated for *Elbow Pain*#
Anatomy
What parts of the elbow are affected?
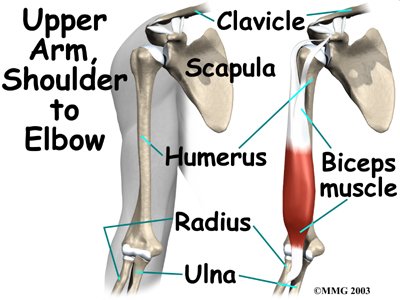
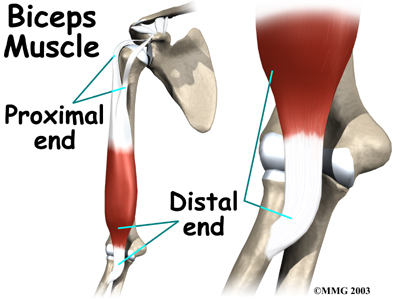
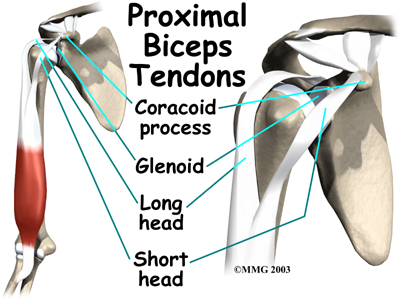
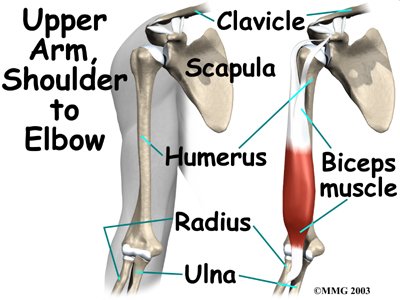
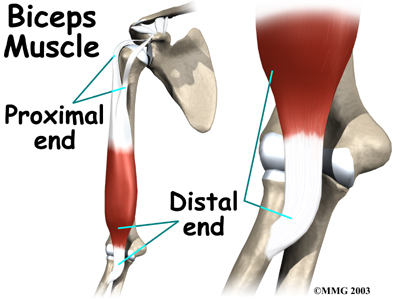
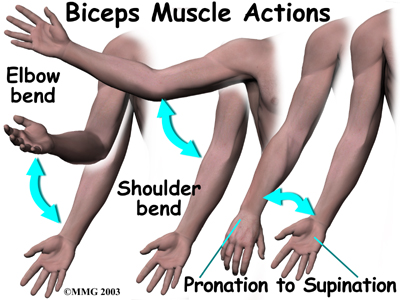
The biceps muscle goes from the shoulder to the elbow on the front of the upper arm. Tendons attach muscles to bone. Two separate tendons connect the upper part of the biceps muscle to the shoulder. One tendon connects the lower end of the biceps to the elbow.
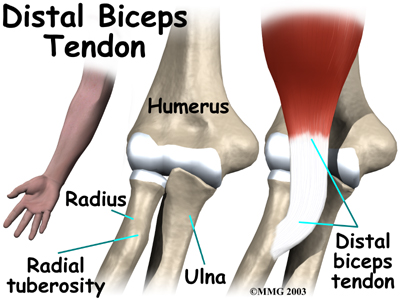
The lower biceps tendon is called the distal biceps tendon. The word distal means that the tendon is further down the arm. The upper two tendons of the biceps are called the proximal biceps tendons, because they are closer to the top of the arm.
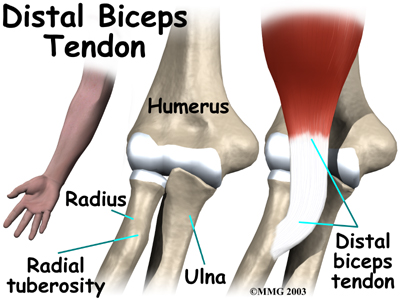
The attaches to a small bump on the radius bone of the forearm. This small bony bump is called the radial tuberosity. The radius is the smaller of the two bones between the elbow and the wrist that make up the forearm. The radius goes from the outside edge of the elbow to the thumb side of the wrist. It parallels the larger bone of the forearm, the ulna. The ulna goes from the inside edge of the elbow to the wrist.
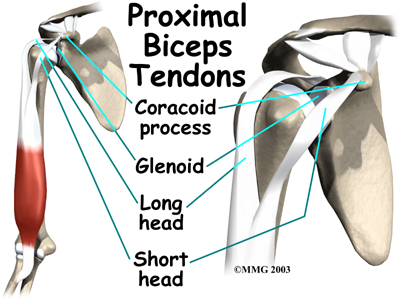
The upper (proximal) end of the biceps has to the shoulder. The main attachment is the long head of the biceps. It connects the biceps muscle to the top of the shoulder socket, called the glenoid. The short head of the biceps angles up and in to its attachment on the corocoid process of the shoulder blade. The corocoid process is a small bony knob in the front of the shoulder.
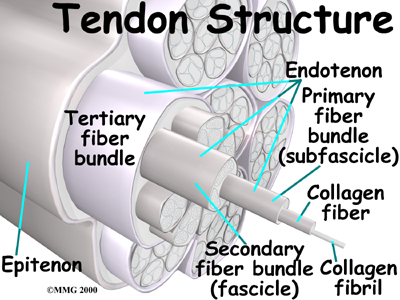
Tendons are made up of strands of a material called . The collagen strands are lined up in bundles next to each other.
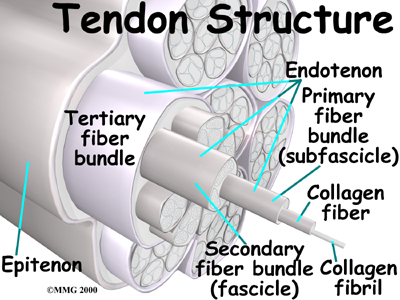
Because the collagen strands in tendons are lined up, tendons have high tensile strength. This means they can withstand high forces that pull on both ends of the tendon. When muscles contract, they pull on one end of the tendon. The other end of the tendon pulls on the bone, causing the bone to move.
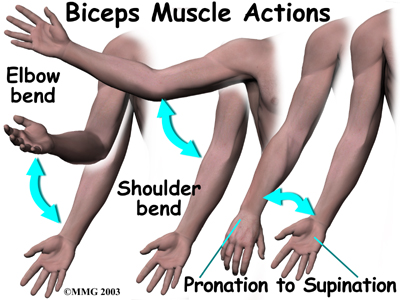
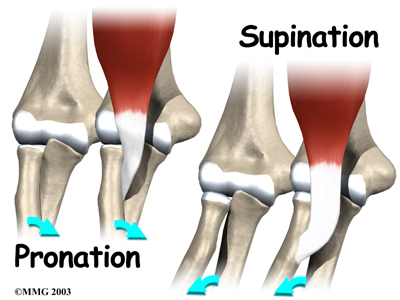
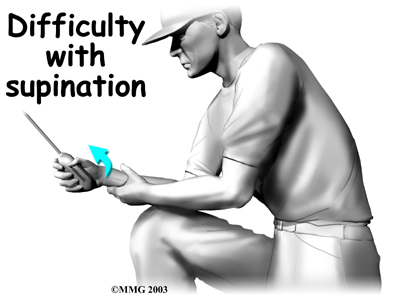
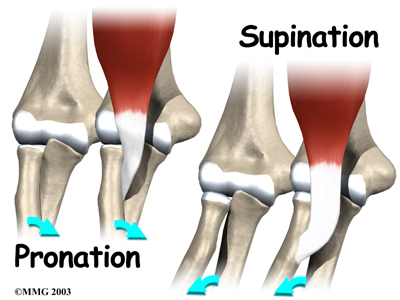
can bend the elbow upward. The biceps can also help flex the shoulder, raising the arm up. And the biceps can rotate, or twist, the forearm in a way that points the palm of the hand up. This movement is called . Supination positions the hand as if you were carrying a tray.
Related Document: In Motion Therapy's Guide to Elbow Anatomy
Elbow Anatomy Introduction
Causes
 Why did I develop a rupture of the distal biceps?
Why did I develop a rupture of the distal biceps?
The most common cause of a distal biceps rupture happens when a middle-aged man lifts a box or other heavy item with his elbows bent. Often the load is heavier than expected, or the load may shift unexpectedly during the lift. This forces the elbow to straighten, even though the biceps muscle is working hard to keep the elbow bent. The biceps muscle contracts extra hard to help handle the load. As tension on the muscle and tendon increases, the distal biceps tendon where it connects to the radius.
Symptoms
What does a ruptured distal biceps feel like?
When the distal biceps tendon ruptures, it usually sounds and feels like a pop directly in front of the elbow. At first the pain is intense. The pain often subsides quickly after a complete rupture because tension is immediately taken off the pain sensors in the tendon. Swelling and bruising in front of the elbow usually develop shortly after the pop. The biceps may appear to have balled up near the elbow. The arm often feels weak with attempts to bend the elbow, lift the shoulder, or twist the forearm into supination (palm up).
The distal biceps tendon sometimes tears only part of the way. When this happens, a pop may not be felt or heard. Instead, the area in front of the elbow may simply be painful, and the arm may feel weak with the same arm movements that are affected in a complete rupture.
Diagnosis
How can I be sure that I’ve ruptured my distal biceps?
An early diagnosis is best. If surgery is needed, people who've ruptured their distal biceps tendon usually have better results when surgery is done soon after the injury.
When you first visit In Motion Therapy, our physical therapist will take a detailed medical history. You will need to answer questions about the mechanism of injury, your pain, how your pain affects you, your regular activities, and past injuries to your elbow.
The physical exam is often most helpful in diagnosing a rupture of the distal biceps tendon. Our physical therapist may position your elbow and forearm to see which movements are painful and weak. By feeling the muscle and tendon, we can often tell if the tendon has ruptured off the bone.
Some patients may be referred to a doctor for further diagnosis. Once your diagnostic examination is complete, the physical therapists at In Motion Therapy have treatment options that will help speed your recovery, so that you can more quickly return to your active lifestyle.
In Motion Therapy provides physical therapist services in Duluth.
Our Treatment
Non-surgical Rehabilitation
At In Motion Therapy, when we treat a ruptured biceps tendon nonsurgically, we generally advise that you avoid heavy arm activity for three to four weeks. As the pain and swelling resolve, it will become safe to begin doing more normal activities.
Our nonsurgical measures may include recommending a sling to rest the elbow. Anti-inflammatory medicine may be suggested to you by your doctor to help ease pain and swelling and to help you get back to activities sooner.
When you begin your physical therapy program at In Motion Therapy, our physical therapist will give you tips how to rest your elbow and how to do your activities without putting extra strain on the joint. Our physical therapist may apply ice and electrical stimulation to ease pain. We will teach you exercises that are used to gradually strengthen other muscles that can help do the work of a normal biceps muscle.
If the tendon is only partially torn, recovery takes longer. Our patients usually need to rest the elbow using a protective splint or sling. As symptoms ease, you will usually begin a carefully progressed rehabilitation program under the supervision of our physical therapists or occupational therapists. The program often involves one to two months of therapy.
When recovery is well under way, your regular visits to In Motion Therapy will end. Although we will continue to be a resource, you will eventually be in charge of doing your exercises as part of an ongoing home program.
Post-surgical Rehabilitation
Rehabilitation takes longer after surgery. Immediately after surgery, your surgeon may cast your elbow for up to six weeks. Some surgeons prefer to use a special range-of-motion brace with careful elbow motion starting within one to two weeks. When you begin your post-surgical physical therapy at In Motion Therapy, our first few sessions may involve ice and electrical stimulation treatments to help control pain and swelling from the surgery. Our physical therapist may also use massage and other types of hands-on treatments to ease muscle spasm and pain.
We will then gradually have you start exercises to improvement movement in the forearm, elbow, and shoulder. You need to be careful to avoid doing too much, too quickly.
Exercises for the biceps muscle are usually avoided until at least four to six weeks after surgery. Our physical therapist may begin by having you do light isometric strengthening exercises. These exercises work the biceps muscle without straining the healing tendon.
At about six weeks, you may be able to start doing more active strengthening. As you progress, our physical therapist will teach you exercises to strengthen and stabilize the muscles and joints of the wrist and hand, elbow, and shoulder. We may recommend other exercises to work your elbow in ways that are similar to your work tasks and sport activities. Our physical therapist will help you find ways to do your tasks that don't put too much stress on your elbow.
Although the time required for recovery is different for every patient, as a guideline you may require therapy for two to three months. It generally takes four to six months to safely begin doing forceful biceps activity. Before your physical therapy sessions end, we will teach you a number of ways to avoid future problems.
In Motion Therapy provides services for physical therapy in Duluth.
Physician Review
When evaluating your condition, your doctor may order X-rays. X-rays are mainly used to find out if there are other injuries in the elbow. Plain X-rays do not show soft tissues like tendons. They will not show a distal biceps rupture unless a small piece of bone got pulled off the radius as the tendon ruptured. This type of injury is called an avulsion fracture.
Your doctor may also order a magnetic resonance imaging (MRI) scan to see if the biceps tendon is only partially torn or if the tendon fully ruptured. An MRI is a special imaging test that uses magnetic waves to create pictures of the elbow in slices. The MRI can also show if there are other problems in the elbow.
Many doctors prefer to treat distal biceps tendon ruptures with surgery. Nonsurgical treatments are usually only used for people who do minimal activities and require minimal arm strength. Nonsurgical treatments are only used if arm weakness, fatigue, and mild deformity aren't an issue. If you are an older individual who can tolerate loss of strength, or if the injury occurs in your nondominanat arm, you and your doctor may decide that surgery is not necessary.
Not having surgery often results in significant loss of strength. Flexion of the elbow is somewhat affected, but supination (which is the motion of twisting the forearm, such as when you use a screwdriver) can be very affected. A distal biceps rupture that is not repaired reduces supination strength by about 50 percent.
Surgery
People who need normal arm strength get best results with surgery to reconnect the tendon right away. Surgery is needed to avoid tendon retraction. When the tendon has been completely ruptured, contraction of the biceps muscle pulls the tendon further up the arm. When the tendon recoils from its original attachment and remains there for a very long time, the surgery becomes harder, and the results of surgery are not as good.
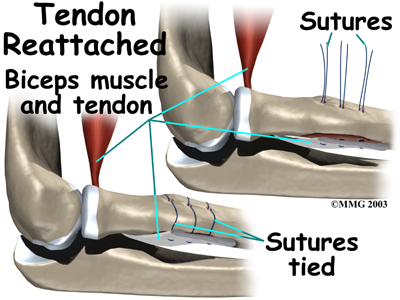
Direct Repair
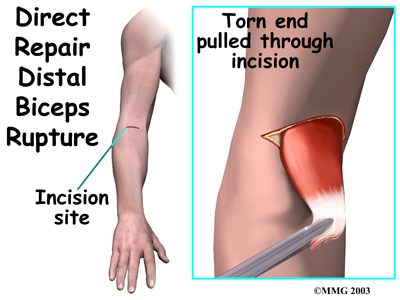
Direct repair surgery is commonly done soon after the rupture. Doing a direct repair soon after the injury lessens the risk of tendon retraction.
In a direct repair, the surgeon begins by making a small incision across the arm, just above the elbow. Forceps are inserted up into this incision to grasp the free end of the ruptured biceps tendon. The surgeon pulls on the forceps to slide the tendon through the incision.
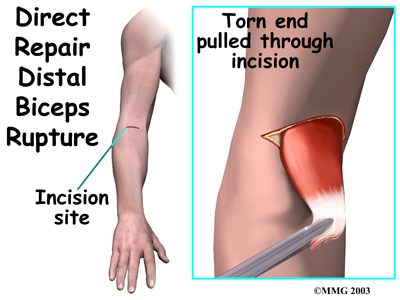
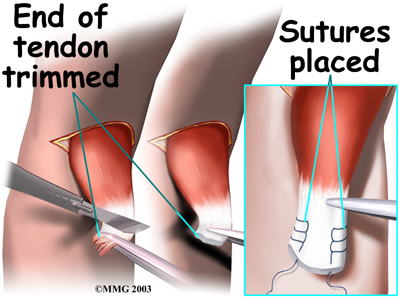
Attention is given to the . A scalpel is used to slice off the damaged and degenerated end. Sutures are then crisscrossed through the bottom inch of the distal biceps tendon.
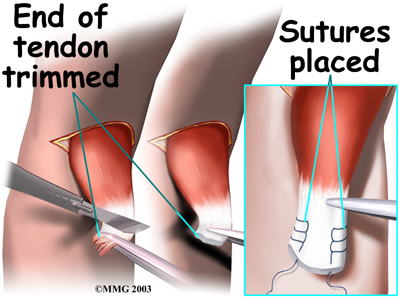
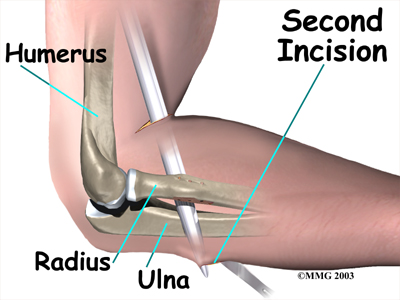
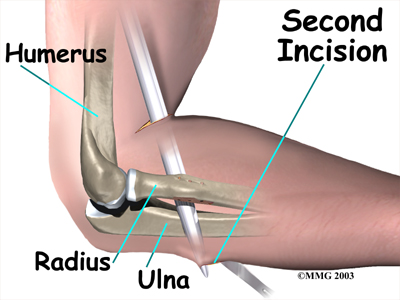
A curved instrument is passed through the incision and directly between the radius and ulna bones. The surgeon pushes the instrument through this space, puncturing the muscles and soft tissues. The surgeon feels the back side of the forearm for the spot where the instrument is protruding. A is made at this spot.
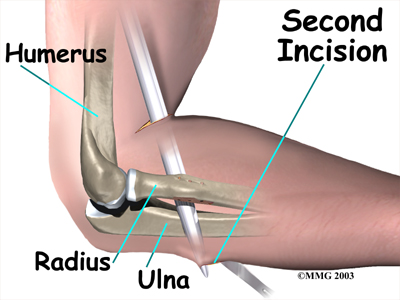
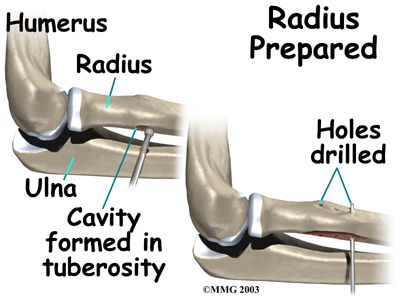
The original attachment on the radius, the radial tuberosity, is . An instrument called a burr shaves off the surface of the tuberosity. The burr is then used to create a small cavity in the bone for the tendon to fit inside. Three small holes are drilled into the top of the rim of bone to secure the sutures.
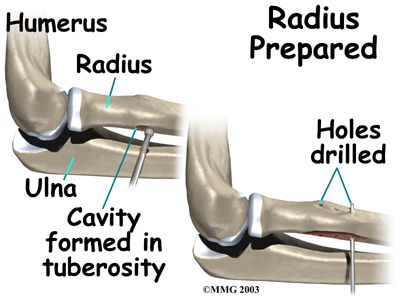
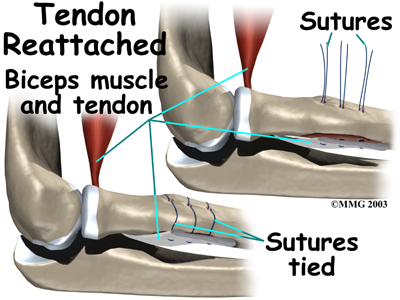
The tendon is passed between the radius and ulna, exiting through the second incision that was made on the back of the forearm. The sutures are threaded into the three holes that were drilled into the rim of the radial tuberosity. The surgeon ties the sutures, securing the . When the surgeon is satisfied with the repair, the skin incisions are closed, and the elbow is placed either in a cast or a range-of-motion brace.
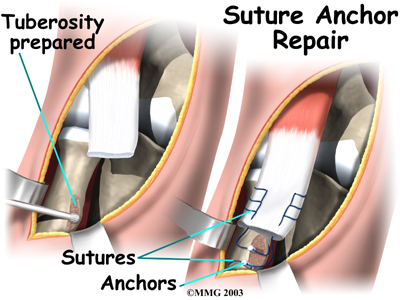
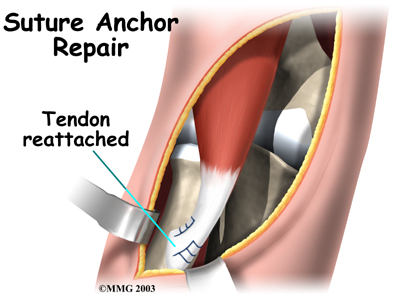
Suture Anchor Method
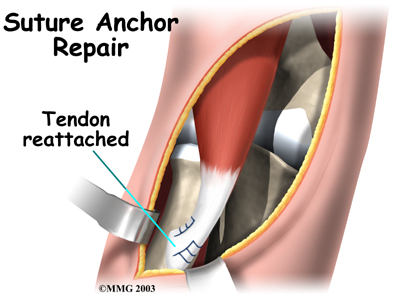 A new method of anchoring the torn tendon to the radius is gaining popularity. This method uses special anchors, called suture anchors, to fix the tendon in place. The procedure requires only one incision and appears to lessen the risk of myositis ossificans. Myositis ossificans is an abnormal healing response that causes bone to form in the muscles and soft tissues.
A new method of anchoring the torn tendon to the radius is gaining popularity. This method uses special anchors, called suture anchors, to fix the tendon in place. The procedure requires only one incision and appears to lessen the risk of myositis ossificans. Myositis ossificans is an abnormal healing response that causes bone to form in the muscles and soft tissues.
The surgeon begins by making a across the arm, just above the elbow. Along the outside edge of the arm, the incision curves and goes upward for a short distance. The skin and underlying tissues are pulled back using retractors. This reveals the front of the lower biceps muscle and allows the surgeon to avoid injuring nearby nerves and arteries. The fascia (connective covering over the muscle) is cut away so the surgeon can see the radial tuberosity.
The original attachment on the radius, the radial tuberosity, is by shaving off the surface with a burr. The burr is then used to create a small cavity in the bone for the tendon to fit inside. Two small suture anchors are embedded into the cavity in the radial tuberosity. These anchors can either be screwed into the bone or implanted like a staple. Each anchor has a long thread (suture) connected to it. The into the lower end of the tendon and crisscrossed upward. The surgeon slides the sutures back and forth, which coaxes the end of the tendon into the cavity. When the end of the tendon is positioned in the cavity, the surgeon tightens the sutures, fixing the tendon in place.
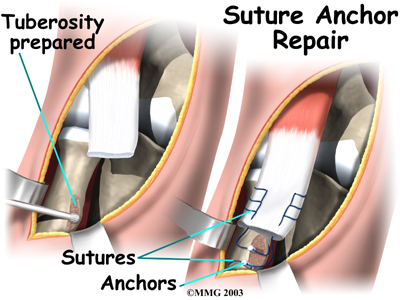
When the surgeon is satisfied with the repair, the skin incisions are closed, and the elbow is placed either in a cast or a range-of-motion brace.
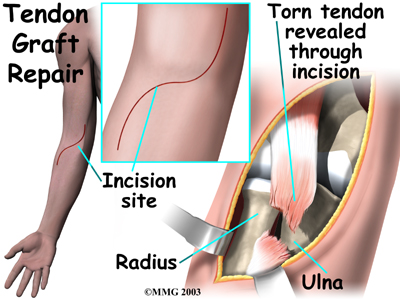
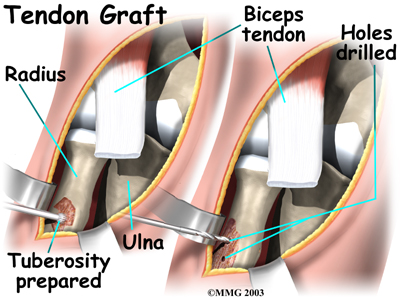
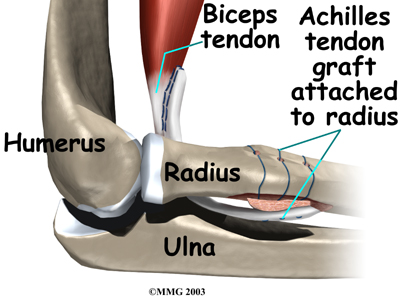
Graft Repair
If more than three or four weeks have passed since the rupture, the surgeon will usually need to make a larger incision in the front of the elbow. Also, because the tendon will have retracted further up the arm, graft tissue will be needed in order to reconnect the biceps to its original point of attachment on the radial tuberosity.
The surgeon begins by making a across the arm, just above the elbow joint. The incision curves along the front surface of the upper arm to expose the lower part of the biceps muscle.
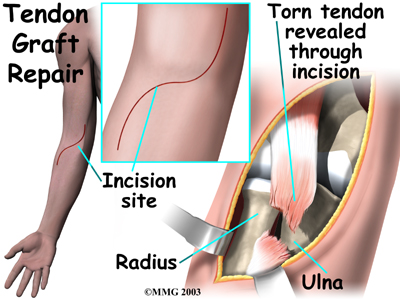
The surface of the is removed. A burr is used to create a small cavity within the tuberosity. Several suture holes are drilled around the rim of the tuberosity.
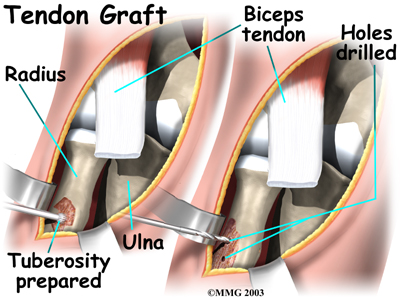
A curved instrument is passed through the incision and directly between the radius and ulna bones. The surgeon pushes the instrument through this space, puncturing the muscles and soft tissues. The surgeon feels the back of the forearm to find the point where the instrument is protruding. A is made at this spot.
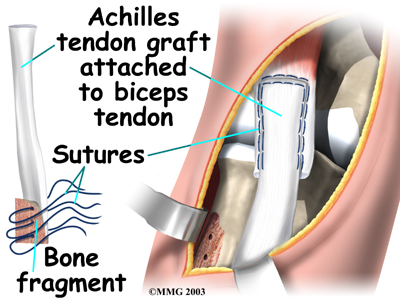
The surgeon then prepares a graft of tissue to lengthen the retracted biceps tendon. Some surgeons use a piece of hamstring tendon for the graft. Others use a section of the Achilles tendon where it attaches to the heel. This type of graft is usually an allograft, meaning that the tissue is taken from a cadaver (human tissue preserved for medical purposes).
When the is used, the surgeon leaves a small piece of the heel bone attached to the piece of tendon. Small holes are drilled into the piece of bone. Sutures are woven through these holes and will later be used to secure the end of the graft to the radial tuberosity. In this way, the graft will have a bone-to-bone connection that heals together. The healed bone solidly fixes the the graft to the radial tuberosity. After the graft is in place, its top end is then stitched over the front of the biceps muscle.
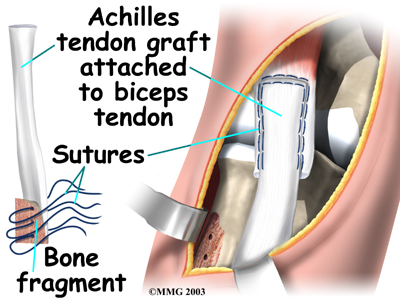
Next, the lower end of the graft is passed between the radius and ulna, exiting through the second incision that was made on the back of the forearm. The sutures from the bony end of the graft are threaded into holes that were drilled into the rim of the radial tuberosity earlier. The surgeon ties the sutures, to the radius.
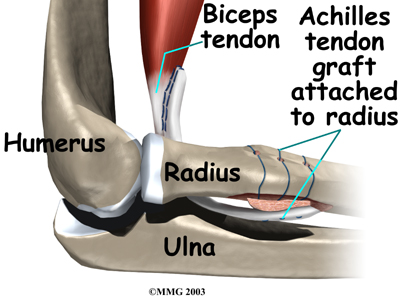
When the surgeon is satisfied with the repair, the skin incisions are closed, and the elbow is placed in a protective brace.
Portions of this document copyright MMG, LLC.


 Why did I develop a rupture of the distal biceps?
Why did I develop a rupture of the distal biceps?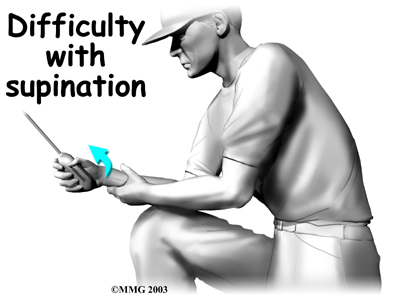
 A new method of anchoring the torn tendon to the radius is gaining popularity. This method uses special anchors, called suture anchors, to fix the tendon in place. The procedure requires only one incision and appears to lessen the risk of myositis ossificans. Myositis ossificans is an abnormal healing response that causes bone to form in the muscles and soft tissues.
A new method of anchoring the torn tendon to the radius is gaining popularity. This method uses special anchors, called suture anchors, to fix the tendon in place. The procedure requires only one incision and appears to lessen the risk of myositis ossificans. Myositis ossificans is an abnormal healing response that causes bone to form in the muscles and soft tissues.