Introduction
Physical therapy in Duluth for Knee Issues
Welcome to In Motion Therapy’s resource on Chondromalacia Patella.
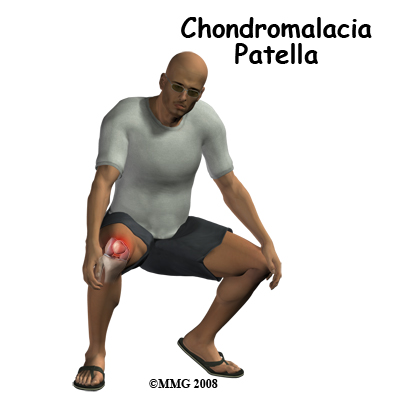
The patella, or kneecap, can be a source of knee pain when it fails to function properly.
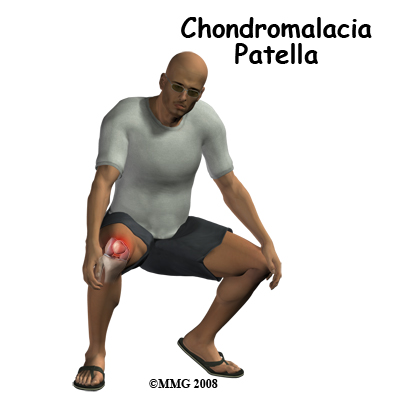
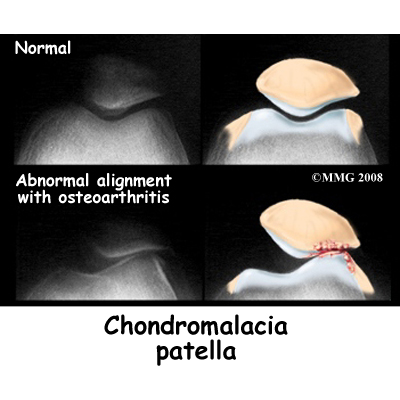
Alignment or overuse problems of the patella can lead to wear and tear of the cartilage behind the patella. Chondromalacia patella is a common knee problem that affects the patella and the groove that the patella slides in over the femur (thigh bone). The kneecap together with the lower end of the femur is considered the patellofemoral joint.
Chondromalacia is the term used to describe a patellofemoral joint that has been structurally damaged, while the term patellofemoral pain syndrome (PFPS) refers to the earlier stages of the condition where structural damage has not yet occurred. Symptoms are more likely to be reversible with PFPS.
This guide will help you understand:
- what parts of the knee are affected
- how this condition develops
- how health care professionals diagnose the condition
- what treatment options are available
- what In Motion Therapy's approach to rehabilitation is
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Knee Pain|limit:15|heading:Hear from some of our patients who we treated for *Knee Pain*#
Anatomy
What is the patella, and what does it do?
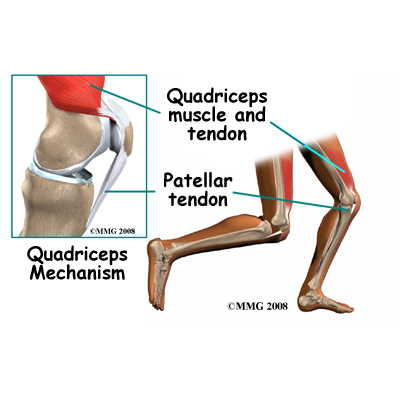
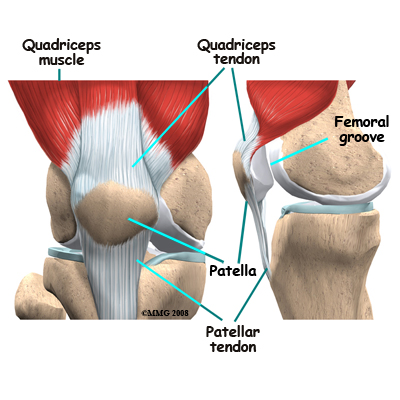
The patella (kneecap) is the moveable bone on the front of the knee. This unique bone is wrapped inside a tendon that connects the large muscles on the front of the thigh, the quadriceps muscles, to the lower leg bone. The large quadriceps tendon together with the patella and patellar ligament is called the extensor mechanism. Though we think of it as a single device, the extensor mechanism has two separate tendons, the quadriceps tendon on top of the patella, which connects the quadriceps muscle to the top of the patella, and the patellar tendon below the patella, which connects the lower portion of the patella to the shinbone (tibia).
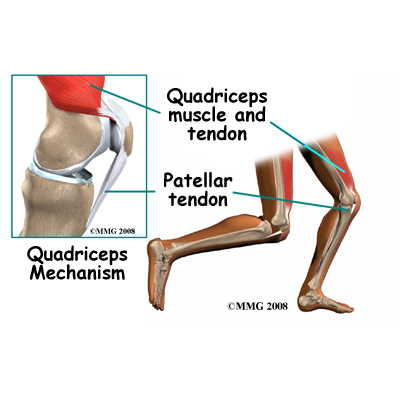
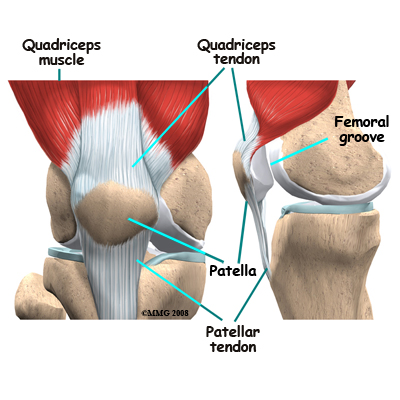
Tightening up the quadriceps muscles places a pull on the tendons of the extensor mechanism. This action causes the knee to straighten. The patella acts like a fulcrum to increase the force of the quadriceps muscles.
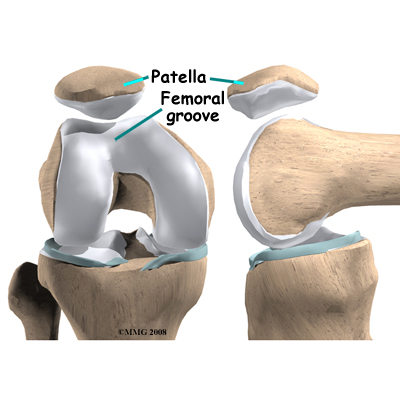
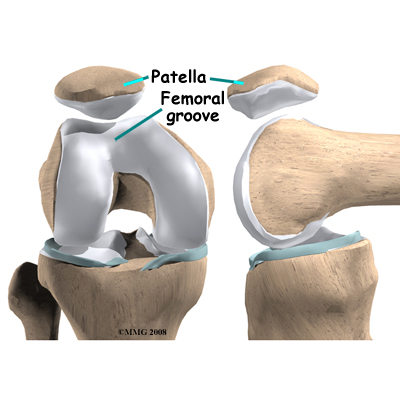
The underside of the patella is covered with articular cartilage, the smooth, slippery covering found on joint surfaces. This covering helps the patella glide (or track) in a special groove made by the thighbone, or femur. This groove is called the femoral groove.
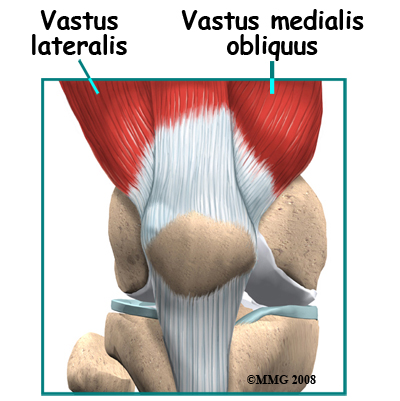
 Two muscles of the thigh attach to the patella and help control its position in the femoral groove as the leg straightens. These two muscles are part of the quadriceps group and are called the vastus medialis obliquus (VMO) and the vastus lateralis (VL). The VMO runs along the inside of the thigh, and the VL lies along the outside of the thigh. If the timing between these two muscles is off or one is stronger than the other then the patella may be pulled off track and rubbing will occur on the articular cartilage on the back of the patella.
Two muscles of the thigh attach to the patella and help control its position in the femoral groove as the leg straightens. These two muscles are part of the quadriceps group and are called the vastus medialis obliquus (VMO) and the vastus lateralis (VL). The VMO runs along the inside of the thigh, and the VL lies along the outside of the thigh. If the timing between these two muscles is off or one is stronger than the other then the patella may be pulled off track and rubbing will occur on the articular cartilage on the back of the patella.
Related Document: In Motion Therapy's Guide to Knee Anatomy
Knee Anatomy Introduction
Causes
What causes this problem?
Problems commonly develop when the patella suffers repetitive wear and tear. The underlying cartilage begins to degenerate, a condition common in young athletes. Soccer players, snowboarders, cyclists, rowers, tennis players, ballet dancers, and runners are often affected but anyone whose knees are under great stress during any work or sport activity is at increased risk of developing chondromalacia patella.
 Wear and tear can develop for several reasons. Both acute injury to the patella, such as a fall, or chronic friction between the patella and the femur, such as during jumping, can generate symptoms of patellofemoral pain syndrome. Degeneration leading to chondromalacia may also develop as part of the aging process, similar to putting a lot of miles on a car, where eventually the car parts wear out.
Wear and tear can develop for several reasons. Both acute injury to the patella, such as a fall, or chronic friction between the patella and the femur, such as during jumping, can generate symptoms of patellofemoral pain syndrome. Degeneration leading to chondromalacia may also develop as part of the aging process, similar to putting a lot of miles on a car, where eventually the car parts wear out.
The main cause of a gradual onset of PFPS, which can lead to chondromalacia patella, is a problem in the way the patella tracks within the femoral groove as the knee moves. Physical and biomechanical changes alter the stress and load on the patellofemoral joint and cause excessive stress on the back of the patella.
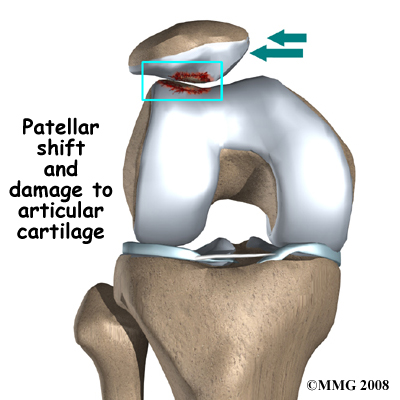
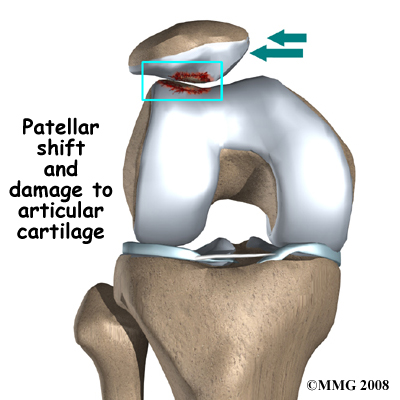
The quadriceps muscle helps control the patella so it stays within the femoral groove. If part of the quadriceps is weak for any reason, a muscle imbalance can occur. When this happens, the pull of the quadriceps muscle may cause the patella to pull more to one side than the other. This in turn causes more pressure on the articular cartilage on one side than the other. In time, this pressure can damage the articular cartilage leading to chondromalacia patella. Muscles that are too tight in the lower extremity, such as the quadriceps muscle itself, or the muscles at the back of the leg or calf (hamstrings and gastrocnemius respectively) can also cause increased pressure on the back of the kneecap leading to early wear and tear.
A similar tracking problem occurs when the timing of the quadriceps muscles is off. As mentioned above, two of the quadriceps muscles that attach to the kneecap control the side-to -side motion. These are the VMO (the muscle running down the inside of the thigh) and the VL (the muscle that runs down the outside part of the thigh.) People with patellofemoral problems sometimes have problems in the timing between the VMO and the VL. Ideally, the smaller VMO fires microseconds earlier than the VL to keep the patella centred. If the VL contracts first it tends to pull the patella toward the outside edge of the knee. The result is abnormal pressure on the articular surface of the patella.
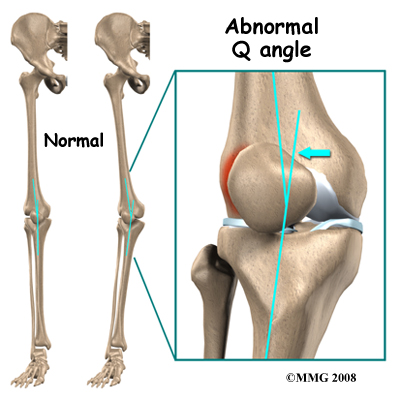 Another type of imbalance may occur due to differences in how the bones of the knee are angled. These differences, or anatomic variations, are something people are born with. The angle between the thighbone and the shinbone is referred to as the "Q angle". Some people are born with a greater than average Q angle. Women also tend to have a greater Q angle than men, due to their wider hips. The patella normally sits at the center of this angle within the femoral groove. When the quadriceps muscle contracts, the knee straightens, pushing the patella slightly to the outside of the knee. In cases where the Q angle is increased, the patella tends to shift outward with greater pressure. This leads to a similar pressure imbalance as when the VL is stronger than the VMO: As the patella slides through the groove, it places more pressure on outside edge of the patella, leading to damage of the underlying articular cartilage.
Another type of imbalance may occur due to differences in how the bones of the knee are angled. These differences, or anatomic variations, are something people are born with. The angle between the thighbone and the shinbone is referred to as the "Q angle". Some people are born with a greater than average Q angle. Women also tend to have a greater Q angle than men, due to their wider hips. The patella normally sits at the center of this angle within the femoral groove. When the quadriceps muscle contracts, the knee straightens, pushing the patella slightly to the outside of the knee. In cases where the Q angle is increased, the patella tends to shift outward with greater pressure. This leads to a similar pressure imbalance as when the VL is stronger than the VMO: As the patella slides through the groove, it places more pressure on outside edge of the patella, leading to damage of the underlying articular cartilage.
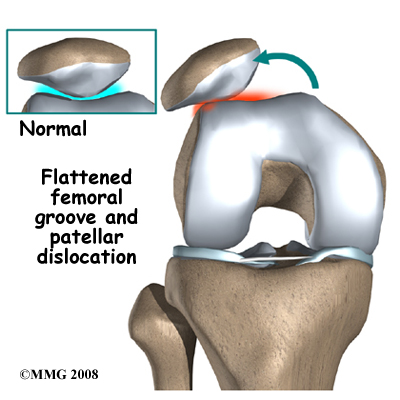
Anatomic variations in the bone shapes themselves can also occur which contribute to the development of chondromalacia patella. For instance, one side of the femoral groove can be smaller than the other. This creates a situation where the groove is too shallow, usually on the outside part of the knee. People who have a shallow groove sometimes have their patella slip sideways out of the groove, causing a patellar dislocation. This is not only painful when it occurs, but it can damage the articular cartilage underneath the patella. If this occurs repeatedly, degeneration of the patellofemoral joint occurs fairly rapidly.
Another anatomic variation can be the patellar position. If the patella sits in an abnormal position, such as quite high or low, it also changes how the patella glides over the femur, and can lead to greater wear and tear on the articular cartilage. In addition, the patella may be very mobile in some individuals. A hypermobile patella does not stay firmly in the femoral groove as the knee straightens and bends so it is at a greater risk of wearing on the cartilage as it moves around, and can possibly skip out of the femoral groove (subluxation or dislocation).
Weakness of the muscles around the hip can also indirectly affect the patella and can lead to patellofemoral joint pain as well as wear and tear on the cartilage of the patella. The muscles of the hip control the position of the knee. A weakness of the muscles that pull the hip out and away from the other leg, or turn the thigh outward (hip abductor and external rotator muscles,) can lead to imbalances in the alignment of the entire leg including the knee joint. This causes abnormal tracking of the patella within the femoral groove and eventually pain around the patella. This misalignment is accentuated when jumping and running, or when descending stairs. Many patients are confused when their physical therapist begins exercises to strengthen and balance the hip muscles, but there is a very good reason that their therapist is focusing on this area.
Finally, the position of the foot plays a large part in maintaining the alignment of the knee and tracking of the patella in the femoral groove. The foot position is also partially controlled by the muscles of the hip and knee, but also by the muscles on the bottom of the foot and the muscles that run from the inside of your shin bone down underneath your foot. If any of these muscles are weak, your arch can drop downwards which causes your knee to rotate inwards. Anatomical variations in the bones of one’s foot may cause flat-footedness, and the result on the knee is the same.
Symptoms
What does chondromalacia patella feel like?
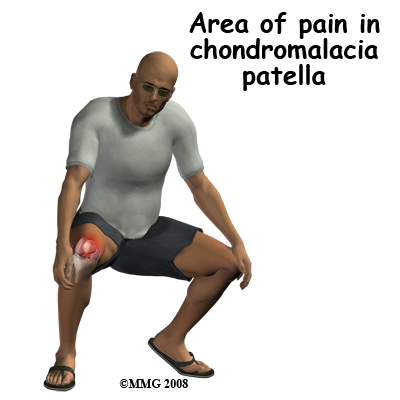 The most common symptom is pain underneath or around the edges of the patella. Often the pain radiates to the medial side of the kneecap whereas others experience vague pain in the knee that isn't centered in any one spot.
The most common symptom is pain underneath or around the edges of the patella. Often the pain radiates to the medial side of the kneecap whereas others experience vague pain in the knee that isn't centered in any one spot.
The pain is made worse by any activities that load the patellofemoral joint, such as running, hill walking, or going up and down stairs. Kneeling or squatting is often too painful to even try. Keeping the knee bent for long periods, such as when sitting in a car or during a movie may also cause pain.
Sometimes there may be a sensation like the patella is slipping or giving way on activities such as jumping or running. Most often this is thought to be a reflex response to pain and not because there is any instability in the kneecap. As mentioned above, however, in some cases where the femoral groove is shallow or the patella is particularly mobile, the patella can sublux, but most often, the reflexive response to pain is to blame for the sensation.
The knee may grind, or you may hear a crunching sound when you squat or go up and down stairs. If there is a considerable amount of wear and tear, you may feel popping or clicking as you bend your knee. These sounds are caused by the uneven surface of the underside of the patella rubbing against the femoral groove. The knee may swell with heavy use and become stiff and tight. This stiffness can be because of fluid accumulating inside the knee joint, sometimes called 'water on the knee'. This swelling is not unique to chondromalacia patella but sometimes occurs when the knee becomes irritated.
Diagnosis
How do health care professionals diagnose the problem?
The history and physical examination are usually enough to suspect the diagnosis of chondromalacia patella. Your physical therapist at In Motion Therapy will question you about your activity level, where precisely the pain is, when the pain began, what you were doing when the pain started, and what movements aggravate or ease the pain. Chondromalacia patella generally begins insidiously (gradual onset) but it can also be instigated by a trauma to the knee, such as a fall onto the kneecap or a hard knock to the knee such as during a collision in sport.
Next your physical therapist will do a physical examination of the knee and entire lower extremities. They will palpate, or touch, around the knee and particularly along the patella to determine the exact location of pain. They will also move your kneecap to determine how mobile it is and may even try to illicit pain by rubbing on the underside of your patella if your patella is mobile enough to allow this. Your physical therapist will look for other factors such as bony alignment (Q-angle,) muscle flexibility, mobility of the patella, and joint laxity that may be contributing to your knee pain. They will want to look at how you stand and your foot position, and may ask to watch you walk, squat, jump or run. Your physical therapist will also check the strength and lengths of the muscles surrounding and affecting the knee joint such as the quadriceps, hamstrings, calves, hip flexors and buttocks muscles. All of these muscles, if weak or tight, can contribute to the forces applied to the knee joint and to the development and ongoing pain of chondromalacia patella.
Your physical therapist will check if they can illicit pain by providing resistance while you straighten your knee. This action generally reproduces the pain associated with chondromalacia patella because it puts pressure on the painful cartilage on the back of the patella and thus helps to confirm the diagnosis.
In Motion Therapy provides services for physical therapy in Duluth.
Physicianís Review
X-rays may be ordered on the initial visit to your doctor. An X-ray can help determine if the patella is properly aligned in the femoral groove. Several X-rays taken with the knee bent at several different angles can help determine if the patella seems to be moving through the femoral groove in the correct alignment. The X-ray may show the wear and tear between the patella and femur, but only when the problem has been there for a while and the wear and tear is significant.
Other tests, such as magnetic resonance imaging (MRI), may be suggested. The MRI machine uses magnetic waves rather than X-rays to show the soft tissues of the body. This machine creates pictures that look like slices of the knee. It used to be that this test was only done to look for injuries such as tears in the menisci or ligaments of the knee but recent advances in the quality of MRI scans have enabled doctors to see the articular cartilage on the scan and determine if it is damaged. This test does not require any needles or special dye and is painless.
In some cases, investigative arthroscopy may be needed to make the definitive diagnosis when there is still a question about whether chondromalacia patella is causing your knee problem. Arthroscopy is an operation that involves placing a small fiber-optic TV camera into the knee joint. This camera allows the surgeon to directly look at the structures inside the joint. They can see the condition of the articular cartilage on the back of your patella from the inside, rather than guessing at the condition of it from the outside. The vast majority of patellofemoral problems are diagnosed without resorting to investigative arthroscopy. Arthroscopy is generally reserved to diagnose knee pain not identified by other means.
Interestingly, there is no clear link between the severity of symptoms and X-ray or arthroscopic findings. This means that you can have severe pain but not much will show up on the investigations. The contrary can also occur; severe damage but little pain. For this reason, most often health care professionals rely upon the history, symptoms, and results of the physical examination to determine chondromalacia patella as the cause of your pain rather than just the results of investigative tests.
Treatment
What treatment options are available?
Nonsurgical Rehabilitation and Treatment
Non-operative treatment is the usual treatment for this problem. You may require 4-6 weeks of physical therapy treatment, and then several more months of a home stretching and strengthening program to treat your chondromalacia patella. Getting the pain and inflammation under control is the first step. The overall goals for a rehab plan are to provide pain relief or pain control, improve muscle function and flexibility, improve knee alignment, and avoid further wear and tear.
The initial treatment for chondromalacia patella at In Motion Therapy will aim to decrease the inflammation and pain in your knee. Simply icing the knee can often assist with the inflammation and relieve a great deal of the pain. In cases of chronic pain (lasting longer than 3 months), heat may be more useful in decreasing pain. Your physical therapist may also use electrical modalities such as ultrasound or interferential current to decrease the pain and inflammation. Massage, particularly for the quadriceps muscle, may also be helpful. During the initial stages of treatment, where the knee is still quite painful, a relative rest from activity may be required. This means that those activities that bother your knee the most may need to be stopped or decreased for a specific amount of time to allow your knee pain to settle down. In many cases, however, you may still be able to partake in a moderate amount of activity. Your physical therapist will advise you on the appropriate amount of rest from activity that will be needed in your specific case. For some patients a complete cessation of all activities is required in order to get the pain and inflammation under control.
Your physician may suggest anti-inflammatory medications, such as aspirin or ibuprofen, as another means of combating the inflammation and pain. Acetaminophen or paracetamol may be suggested for pain control if you can't take anti-inflammatory medications for any reason.
Once the initial pain and inflammation has calmed down, your physical therapist will focus on improving the flexibility, strength, and alignment around the knee joint and entire lower extremity. Static stretches for the muscles and tissues around the knee (particularly the quadriceps and iliotibial band on the outside of the knee) will be prescribed by your physical therapist early on in your treatment to improve flexibility. Again, any tightness in the muscles or tissues around the knee can increase the pull on the patella and affect alignment during walking, running or jumping so it is important to address this immediately.
Strength imbalances will also affect the alignment of the knee and can cause muscles to tighten which put more pressure on the knee and can contribute to the cause of chondromalacia patella. Your physical therapist will determine which muscles in your individual case require the most strengthening. Strength in both the knee and the hip (which controls the knee position) are very important. In most cases your physical therapist will prescribe exercises that strengthen the medial quadriceps muscle (VMO) as this muscle is prone to weakness around the knee, and as described above, when it is not strong enough, the pressure behind the kneecap increases. Your physical therapist will also focus on the particular timing of contraction of this muscle to ensure that it fires when needed to guide the patella properly along the femoral groove.
The muscles of the hip (gluteals) that work to align the knee over top of the foot also have a tendency to be weak so specific attention will be paid to them in the rehabilitation process.
When you have gained enough strength in the knee and hip muscles, your physical therapist will incorporate advanced exercises that force the knee and hip to recruit the correct muscles while under tension and at a quicker rate. When bending the knee in activities such as running, jumping or stair climbing and descending, the knee muscles and ligaments are placed under load while they are stretching (eccentric load.) This load can be tremendous and translates to heavy loads on the back of the kneecap. In order to prepare the patella to take this load once you return to activity your physical therapist will prescribe ‘eccentric’ muscle strengthening. Bending the knee quickly into a squatting position and then stopping rapidly (drop squats) encourages the patella (and entire knee joint) to adapt to the force that will eventually be needed to return to physical activity, and to recruit the proper muscles with the proper timing. When appropriate, weights can be added to simulate the increased body weight that the knee endures during running and jumping. Your physical therapist may ask you to do this exercise on a board slanting downwards (approximately 25 degrees) which has been shown to improve the recruitment of the required knee muscles. In addition, an electrical muscle stimulator may be used on the quadriceps muscle during the activity, which encourages improved recruitment of the muscle, particularly the VMO. All exercises should be completed with minimal or no pain and advancing the exercises should be done only at the discretion of your physical therapist. Once these exercise are mastered, your physical therapist may add even more advanced jumping and landing exercises from a height or on different surfaces.
As part of your treatment your physical therapist may use a hands-on technique to mobilize your kneecap and improve its flexibility if it is stiff. In cases where the patella does not move well, improved movement can assist in decreasing the resistance that the VMO needs to work against and make tracking of the patella easier to control.
Taping the kneecap may also help you to do exercises and activities with less pain. Your physical therapist may even teach your how to tape your own knee so you can do it for sporting activities that you are still engaging in. Taping over a longer time frame will cause irritation to the skin and can be cumbersome, therefore if the taping helps, a brace, which performs a similar function, may be suggested. Braces used for chondromalacia patella are made of soft fabric, such as cloth or neoprene, and work to encourage proper alignment of the patella as it glides down the knee. There are small buttress pads in the brace that sit on the side of the patella to keep it lined up within the groove of the femur. Patients commonly report less pain and improved function with both taping and bracing.
As mentioned above, proper alignment of your entire lower extremity is paramount to decreasing the overall stress that is placed on the patella and knee in general. In addition to strengthening, stretching, hands-on treatment, and taping, foot orthotics may be useful to assist with alignment. Strengthening of the muscles of the shin and foot can help with the foot alignment, but often this is not enough to fully correct the problem, and foot orthotics are required. Alignment of the foot in turn then encourages proper alignment up the lower extremity chain. Your physical therapist can advise you on whether orthotics would be useful for you, and also on where to purchase them.
A critical part of our treatment for chondromalacia patella at In Motion Therapy includes specific education on returning to full physical activity. Bending and straightening the knee occurs often even in everyday activities such as walking or stair climbing so a patella that is recovering from injury can easily be aggravated. Returning you back to normal physical activity at a graduated pace is crucial to avoid repetitive pain or a chronic injury. Your physical therapist will advise you on the acceptable level of activity at each stage of your rehabilitation process and assist you in returning to your activities as quickly but as safely as possible.
With a well-planned rehabilitation program and adherence to suggested levels of rest and activity modification, most people respond very well to the treatment we provide for chondromalacia patella at In Motion Therapy. If, however, your knee pain is not responding to the treatment then we may suggest that you consult an orthopaedic surgeon as surgery may be necessary in your case to resolve your pain.
In Motion Therapy provides services for physical therapy in Duluth.
Surgery
If nonsurgical treatment fails to improve your condition, surgery may be suggested. The procedure used for patellofemoral problems varies. In severe cases a combination of one or more of the following procedures may be necessary.
Arthroscopic Method
Arthroscopy is sometimes useful in the treatment of patellofemoral problems of the knee. Looking directly at the articular cartilage surfaces of the patella and the femoral groove is the most accurate way of determining how much wear and tear there is in these areas. Your surgeon can also watch as the patella moves through the groove, and may be able to decide whether or not the patella is moving normally. If there are areas of articular cartilage damage behind the patella that are creating a rough surface, special tools can be used by the surgeon to smooth the surface and reduce your pain. This procedure is sometimes referred to as ‘shaving the patella.’
Cartilage Procedure
In more advanced cases of patellar arthritis, surgeons may operate to repair or restore the damaged cartilage. The type of surgery needed to repair articular cartilage is based on the size, type, and location of the damage. Along with surgical treatment to fix the cartilage, other procedures may also be done to help align the patella so less pressure is placed on the healing cartilage.
Lateral Release
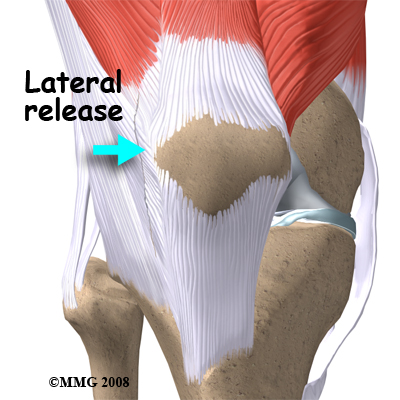 If your patella problems appear to be caused by a misalignment problem, a procedure called a lateral release may be suggested. This procedure is done to allow the patella to shift back to a more normal position and relieve pressure on the articular cartilage. In this operation, the tight ligaments on the outside (lateral side) of the patella are cut, or released, to allow the patella to slide more towards the center of the femoral groove. These ligaments eventually heal with scar tissue that fills in the gap created by the surgery, but they no longer pull the patella to the outside as strongly as prior to the surgery. This helps to balance the pull from the quadriceps muscles and equalize the pressure on the articular cartilage behind the patella.
If your patella problems appear to be caused by a misalignment problem, a procedure called a lateral release may be suggested. This procedure is done to allow the patella to shift back to a more normal position and relieve pressure on the articular cartilage. In this operation, the tight ligaments on the outside (lateral side) of the patella are cut, or released, to allow the patella to slide more towards the center of the femoral groove. These ligaments eventually heal with scar tissue that fills in the gap created by the surgery, but they no longer pull the patella to the outside as strongly as prior to the surgery. This helps to balance the pull from the quadriceps muscles and equalize the pressure on the articular cartilage behind the patella.
Ligament Tightening Procedure
In some cases of severe patellar misalignment, a lateral release alone may not be enough. For problems of repeated patellar dislocations, the tendons on the inside edge of the knee (the medial side) may have to be tightened as well.
Bony Realignment
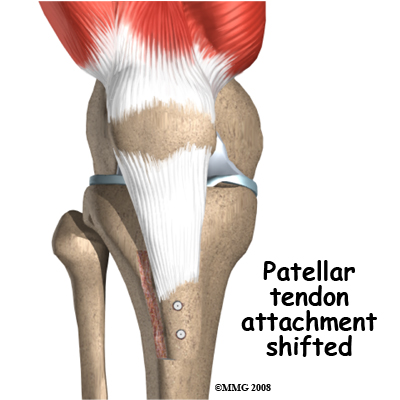 If the misalignment is severe, the bony attachment of the patellar tendon may also have to be shifted to a new spot on the tibia (shin bone.) Remember that the patellar tendon attaches the patella to the tibia just below the knee. By moving a section of bone where the patellar tendon attaches to the tibia, surgeons can change the way the tendon pulls the patella through the femoral groove.
If the misalignment is severe, the bony attachment of the patellar tendon may also have to be shifted to a new spot on the tibia (shin bone.) Remember that the patellar tendon attaches the patella to the tibia just below the knee. By moving a section of bone where the patellar tendon attaches to the tibia, surgeons can change the way the tendon pulls the patella through the femoral groove.
The surgeon removes a section of bone where the patellar tendon attaches on the tibia. This section of bone is then reattached on the tibia closer to the other knee.
Usually, the bone is reattached onto the tibia using screws. This procedure shifts the patella to the medial side. Once the surgery heals, the patella should track better within the center of the groove, spreading the pressure equally on the articular cartilage behind the patella.
Arthroscopic procedures to shave the patella or a simple lateral release can usually be done on an outpatient basis, meaning you can leave the hospital the same day. If your problem requires the more involved surgical procedure where bone must be cut to move the patellar tendon attachment, you may need to spend one or two nights in the hospital.
Post Surgical Rehabilitation
Patients undergoing a patellar shaving usually begin rehabilitation at In Motion Therapy right away. More involved surgeries for patellar realignment or restorative procedures for the articular cartilage may require a delay before starting at In Motion Therapy just to give the tissues a short time to begin the healing process before they are stressed. Rehabilitation will be slower with a realignment or restorative procedure as the bone and cartilage needs more time to heal before too much strain can be put on the knee.
Your first few appointments at In Motion Therapy will focus on helping to control the pain and swelling from the surgery. Icing the knee frequently will assist with the inflammation and relieve a great deal of the pain. Your physical therapist may also use electrical modalities such as ultrasound or interferential current to decrease the pain and inflammation. Massage, particularly for the quadriceps muscle, may also be helpful in the early stages after surgery.
One of the first exercises your physical therapist will prescribe will be some gentle range of motion exercises for your knee to gradually regain full movement. This should be done within a pain free range of motion, however, movement will be encouraged even if it causes a slight bit of discomfort as the movement itself can greatly assist with dispersing any inflammation as well as improving the overall level of pain. A stationary bicycle can be very useful in the initial stages of gaining range of motion in the knee, so if able, you will be encouraged to use one. Even if you are unable to fully rotate the pedals, the back and forth motion on the bike is an excellent method of slowly encouraging the knee to regain its full range of motion.
Your physical therapist will begin to add some gentle strengthening exercises as well for your knee. Initially these may only involve isometric exercises, where you tighten and hold the quadriceps muscle without actually moving the knee itself. Gradually though, the strengthening exercises will be advanced and will address any deficits in strength that your physical therapist has identified as contributing factors to the initial development of your chondromalacia patella.
As you recover from the direct effects of the surgery, your physical therapist will begin to add in exercises to your program similar to that listed under non-surgical rehabilitation. Flexibility of the knee and hip will be addressed, as well as the strength, and the overall alignment of these joints during your rehabilitation exercises and everyday activities. Eccentric exercises will be added as soon as they are appropriate, and exercises specific to the sport you enjoy will also be incorporated as soon as it is safe to do so
When you are well under way with your rehabilitation, regular visits to In Motion Therapy will end. Your physical therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program. Generally rehabilitation at In Motion Therapy after surgery for chondromalacia patella goes extremely well and clients can return without difficulties to the activities they enjoy participating in. If however, your pain is lasting longer that your therapist thinks it should or you are not progressing as rapidly as we would expect, we will ask you to follow up with your surgeon to ensure that there are no complicating factors impeding your rehabilitation.
In Motion Therapy provides services for physical therapy in Duluth.
Portions of this document copyright MMG, LLC.


 Two muscles of the thigh attach to the patella and help control its position in the femoral groove as the leg straightens. These two muscles are part of the quadriceps group and are called the vastus medialis obliquus (VMO) and the vastus lateralis (VL). The VMO runs along the inside of the thigh, and the VL lies along the outside of the thigh. If the timing between these two muscles is off or one is stronger than the other then the patella may be pulled off track and rubbing will occur on the articular cartilage on the back of the patella.
Two muscles of the thigh attach to the patella and help control its position in the femoral groove as the leg straightens. These two muscles are part of the quadriceps group and are called the vastus medialis obliquus (VMO) and the vastus lateralis (VL). The VMO runs along the inside of the thigh, and the VL lies along the outside of the thigh. If the timing between these two muscles is off or one is stronger than the other then the patella may be pulled off track and rubbing will occur on the articular cartilage on the back of the patella.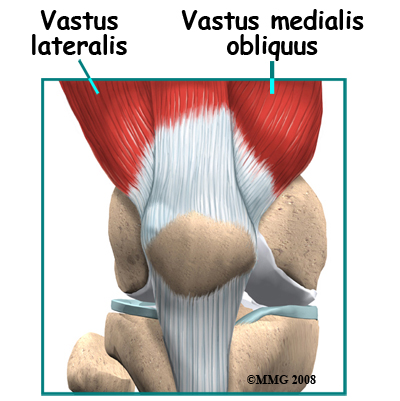
 Wear and tear can develop for several reasons. Both acute injury to the patella, such as a fall, or chronic friction between the patella and the femur, such as during jumping, can generate symptoms of patellofemoral pain syndrome. Degeneration leading to chondromalacia may also develop as part of the aging process, similar to putting a lot of miles on a car, where eventually the car parts wear out.
Wear and tear can develop for several reasons. Both acute injury to the patella, such as a fall, or chronic friction between the patella and the femur, such as during jumping, can generate symptoms of patellofemoral pain syndrome. Degeneration leading to chondromalacia may also develop as part of the aging process, similar to putting a lot of miles on a car, where eventually the car parts wear out.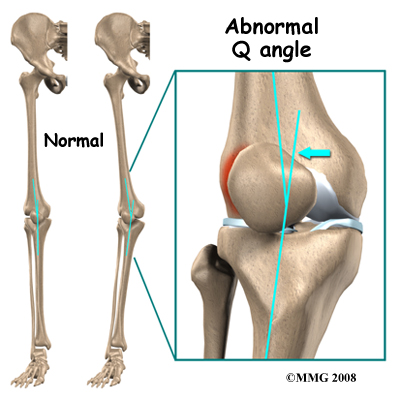 Another type of imbalance may occur due to differences in how the bones of the knee are angled. These differences, or anatomic variations, are something people are born with. The angle between the thighbone and the shinbone is referred to as the "Q angle". Some people are born with a greater than average Q angle. Women also tend to have a greater Q angle than men, due to their wider hips. The patella normally sits at the center of this angle within the femoral groove. When the quadriceps muscle contracts, the knee straightens, pushing the patella slightly to the outside of the knee. In cases where the Q angle is increased, the patella tends to shift outward with greater pressure. This leads to a similar pressure imbalance as when the VL is stronger than the VMO: As the patella slides through the groove, it places more pressure on outside edge of the patella, leading to damage of the underlying articular cartilage.
Another type of imbalance may occur due to differences in how the bones of the knee are angled. These differences, or anatomic variations, are something people are born with. The angle between the thighbone and the shinbone is referred to as the "Q angle". Some people are born with a greater than average Q angle. Women also tend to have a greater Q angle than men, due to their wider hips. The patella normally sits at the center of this angle within the femoral groove. When the quadriceps muscle contracts, the knee straightens, pushing the patella slightly to the outside of the knee. In cases where the Q angle is increased, the patella tends to shift outward with greater pressure. This leads to a similar pressure imbalance as when the VL is stronger than the VMO: As the patella slides through the groove, it places more pressure on outside edge of the patella, leading to damage of the underlying articular cartilage.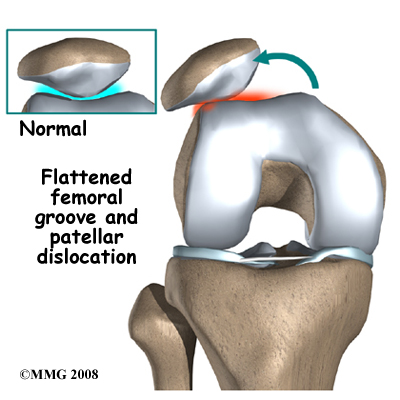
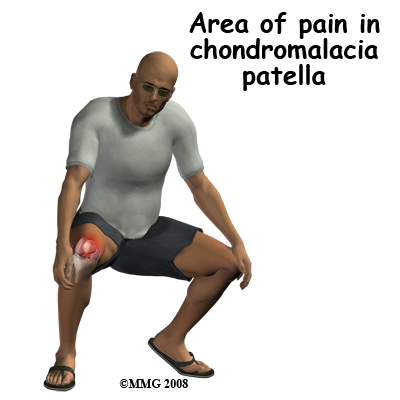 The most common symptom is pain underneath or around the edges of the patella. Often the pain radiates to the medial side of the kneecap whereas others experience vague pain in the knee that isn't centered in any one spot.
The most common symptom is pain underneath or around the edges of the patella. Often the pain radiates to the medial side of the kneecap whereas others experience vague pain in the knee that isn't centered in any one spot.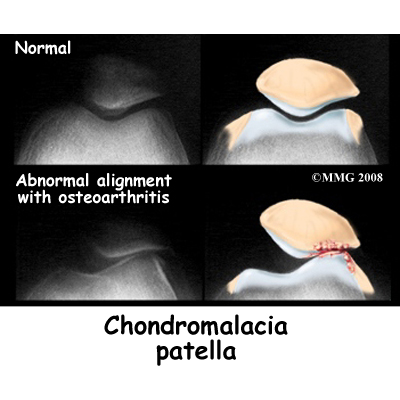
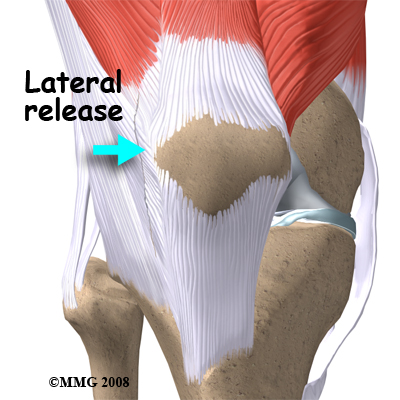 If your patella problems appear to be caused by a misalignment problem, a procedure called a lateral release may be suggested. This procedure is done to allow the patella to shift back to a more normal position and relieve pressure on the articular cartilage. In this operation, the tight ligaments on the outside (lateral side) of the patella are cut, or released, to allow the patella to slide more towards the center of the femoral groove. These ligaments eventually heal with scar tissue that fills in the gap created by the surgery, but they no longer pull the patella to the outside as strongly as prior to the surgery. This helps to balance the pull from the quadriceps muscles and equalize the pressure on the articular cartilage behind the patella.
If your patella problems appear to be caused by a misalignment problem, a procedure called a lateral release may be suggested. This procedure is done to allow the patella to shift back to a more normal position and relieve pressure on the articular cartilage. In this operation, the tight ligaments on the outside (lateral side) of the patella are cut, or released, to allow the patella to slide more towards the center of the femoral groove. These ligaments eventually heal with scar tissue that fills in the gap created by the surgery, but they no longer pull the patella to the outside as strongly as prior to the surgery. This helps to balance the pull from the quadriceps muscles and equalize the pressure on the articular cartilage behind the patella.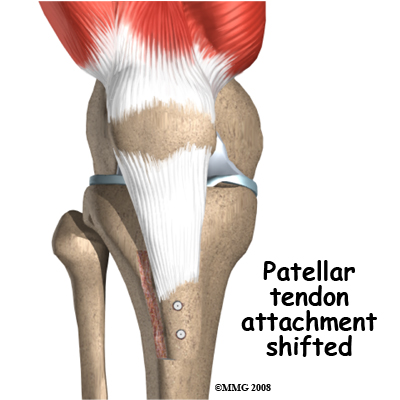 If the misalignment is severe, the bony attachment of the patellar tendon may also have to be shifted to a new spot on the tibia (shin bone.) Remember that the patellar tendon attaches the patella to the tibia just below the knee. By moving a section of bone where the patellar tendon attaches to the tibia, surgeons can change the way the tendon pulls the patella through the femoral groove.
If the misalignment is severe, the bony attachment of the patellar tendon may also have to be shifted to a new spot on the tibia (shin bone.) Remember that the patellar tendon attaches the patella to the tibia just below the knee. By moving a section of bone where the patellar tendon attaches to the tibia, surgeons can change the way the tendon pulls the patella through the femoral groove.