Introduction
Physical therapy in Duluth for Knee
Welcome to In Motion Therapy's guide to Quadriceps Tendonitis.
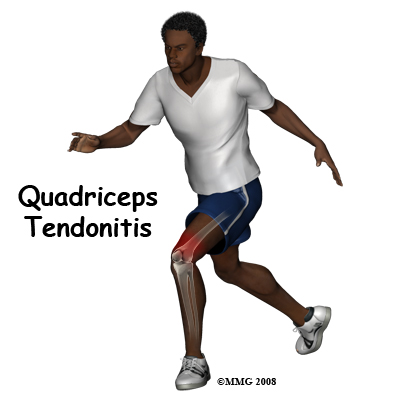
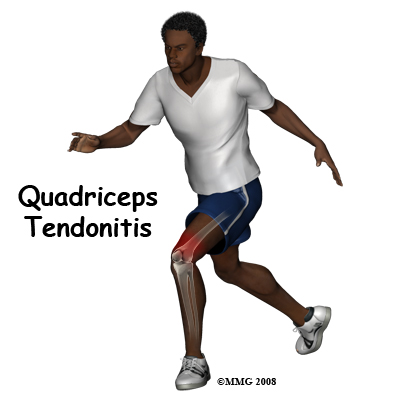 Alignment or overuse problems of the knee structures can lead to strain, irritation, and/or injury of the quadriceps muscle and tendon. This produces pain, weakness, and swelling of the knee joint.
Alignment or overuse problems of the knee structures can lead to strain, irritation, and/or injury of the quadriceps muscle and tendon. This produces pain, weakness, and swelling of the knee joint.
These problems can affect people of all ages but the majority of patients with overuse injuries of the knee (and specifically quadriceps tendonitis) are involved in sports such as soccer, volleyball, running activities, or other repetitive jumping activities.
This guide will help you understand:
- how the problem develops
- how health care professionals diagnose the condition
- what treatment options are available
- what In Motion Therapy’s approach to rehabilitation is
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Knee Pain|limit:15|heading:Hear from some of our patients who we treated for *Knee Pain*#
Anatomy
What is the quadriceps muscle/tendon, and what does it do?
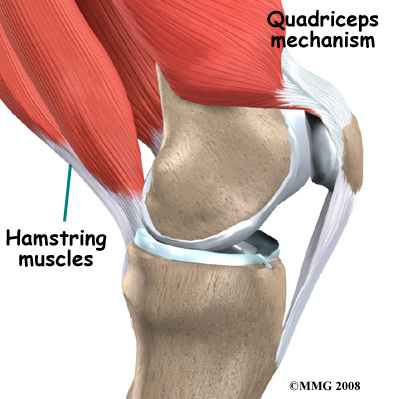
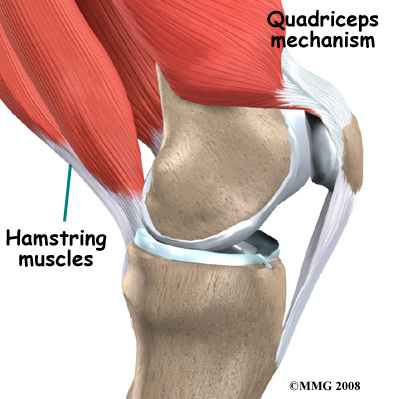 The patella (kneecap) is the moveable bone on the front of the knee. This unique bone is wrapped inside a tendon that connects the large muscles on the front of the thigh, the quadriceps muscles, to the lower leg bone.
The patella (kneecap) is the moveable bone on the front of the knee. This unique bone is wrapped inside a tendon that connects the large muscles on the front of the thigh, the quadriceps muscles, to the lower leg bone.
The large quadriceps muscle ends in a tendon that inserts into the tibial tubercle, a bony bump at the top of the tibia (shin bone) just below the patella. The quadriceps tendon (on the top of the patella) together with the patella and the patellar tendon (on the bottom of the patella) is called the quadriceps mechanism.
Tightening up the quadriceps muscles places a pull on the tendons of the quadriceps mechanism. This action causes the knee to straighten. The patella acts like a fulcrum to increase the force of the quadriceps muscles.
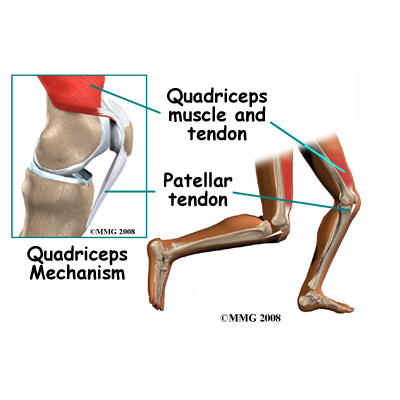
The long bones of the femur and the tibia act as lever arms, placing force or load on the knee joint and surrounding soft tissues. The amount of load can be quite significant. For example, the joint reaction forces of the lower extremity (including the knee) are two to three times the body weight during walking and up to five times the body weight when running.
Related Document: In Motion Therapy's Guide to Knee Anatomy.
Knee Anatomy Introduction
Causes
How does this problem develop?
Quadriceps tendonitis occurs most often as a result of repetitive stresses placed on the supporting structures of the knee. Running, jumping, and quick starts and stops contribute to this condition. Overuse injuries from sports activities are the most common causes of quadriceps tendonitis but anyone can be affected, even those who do not participate in sports or recreational activities.
There are both extrinsic factors (those not related to the body) and intrinsic factors (those pertaining to the body) that can contribute to the development of quadriceps tendonitis. Extrinsic factors include inappropriate footwear, training errors such as doing too much too quickly, or for too long, and inappropriate sport training/playing ground being used.
Intrinsic factors such as age, flexibility, and joint laxity are also important. Misalignment of the foot, ankle, and leg can play a key role in tendonitis. Factors such as a flat foot position, tracking abnormalities of the patella, rotation of the tibia, and a leg length difference can create increased and often uneven load on the quadriceps mechanism. Any muscle imbalance of the lower extremity (from the hip down to the toes) can impact the quadriceps muscle and affect the joint. Individuals who are overweight may have added issues with load and muscle imbalance leading to quadriceps tendonitis.
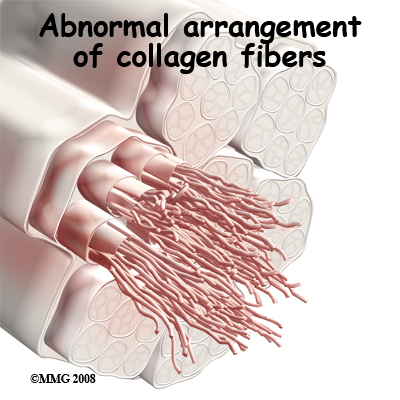 Strength of the patellar tendon is in direct proportion to the number, size, and orientation of the collagen fibers that make up the tendon. Overuse is simply a mismatch between load or stress on the tendon and the ability of that tendon to distribute the force. If the forces placed on the tendon are greater than the strength of the structure, then injury can occur. Repeated microtrauma at the musculotendinous junction may overcome the tendon's ability to heal itself. As a result issue breakdown occurs triggering an inflammatory response that leads to tendonitis and even partial tears.
Strength of the patellar tendon is in direct proportion to the number, size, and orientation of the collagen fibers that make up the tendon. Overuse is simply a mismatch between load or stress on the tendon and the ability of that tendon to distribute the force. If the forces placed on the tendon are greater than the strength of the structure, then injury can occur. Repeated microtrauma at the musculotendinous junction may overcome the tendon's ability to heal itself. As a result issue breakdown occurs triggering an inflammatory response that leads to tendonitis and even partial tears.
Chronic quadriceps overuse leads to a problem called tendonosis. Unlike with tendonitis, inflammation is not present in tendonosis. Instead, degeneration and/or scarring of the tendon has developed due to long-term wear and tear. Chronic tendon injuries are much more common in older athletes (30 to 50 years old).
Symptoms
What does quadriceps tendonitis feel like?
Pain from quadriceps tendonitis is felt in the area at the bottom of the thigh, just above the patella. The pain is most noticeable when you move your knee. The more you move your knee, the more tenderness develops in the area.
There may be swelling in and around the quadriceps tendon and the tendon may be tender or very sensitive to touch. You may feel a sense of warmth or burning pain. The pain can be mild or in some cases the pain can be severe enough to keep the runner from running or other athletes from participating in their sport. Stiffness of the knee is common when you first get up in the morning (or after a long period of rest or inactivity), as well as during and after exercise.
Diagnosis
How do health care professionals diagnose the problem?
Diagnosis begins with a complete history of your knee problem followed by an examination of the knee, including the patella. Your physical therapist at In Motion Therapy will ask you questions about where precisely the pain is, when the pain began, what you were doing when the pain started, and what movements aggravate or ease the pain. As mentioned above, extrinsic factors such as training history as well as type of footwear are important for your therapist to inquire about. The history alone will often lead your physical therapist to the suspicion of quadriceps tendonitis.
Next your physical therapist will do a physical examination of the knee and entire lower extremities. They will palpate, or touch, around the knee and particularly along the quadriceps tendon to determine the exact location of pain. Your physical therapist will look for the individual intrinsic factors mentioned above, such as alignment and flexibility that may be affecting your knee. They will assess the stability of the knee joint to determine if the laxity of the ligaments and tissues surrounding the knee joint are contributing to the problem.
Your physical therapist may want to look at how you stand, your foot position, or watch you walk, squat, or jump. Your physical therapist will also check the strength and lengths of the muscles surrounding and affecting the knee joint such as the quadriceps, hamstrings, calves, hip flexors and buttocks muscles. All of these muscles, if weak or tight, can contribute to the forces applied to the knee joint and lead to the development of quadriceps tendonitis. Providing resistance while you straighten your knee generally reproduces the pain associated with quadriceps tendonitis so this will also be tested. Weakness during this straightening motion or on squatting on one leg may cause your physical therapist to suspect a partially torn or ruptured quadriceps tendon. Often a divot in the contour of the tendon can be felt if the tendon is even partially torn and an investigative exam is generally then done to confirm the diagnosis.
Diagnostic Tests
X-rays may be ordered on the initial visit to your doctor. An X-ray can show fractures or the presence of calcium deposits in the quadriceps muscle but X-rays do not show soft tissue injuries. If a soft tissue injury is suspected, such as a quadriceps tendon tear or rupture, other tests, such as ultrasonography or magnetic resonance imaging (MRI), may be required. Ultrasound uses sound waves to detect tendon tears. MRIs use magnetic waves rather than X-rays to show the soft tissues of the body. An MRI machine creates pictures that look like slices of the knee. This test does not require any needles or special dye and is painless.
In Motion Therapy provides services for physical therapy in Duluth.
Treatment
What treatment options are available?
Nonsurgical Rehabilitation
Quadriceps tendonitis is usually self-limiting. That means the condition will run its course and resolve with the appropriate rest, activity modification, and physical therapy. Recurrence of the problem is common for patients who fail to let the quadriceps tendon recover fully before resuming training or other aggravating activities.
The initial aim of treatment for acute quadriceps tendonitis at In Motion Therapy is to decrease the inflammation and pain in the knee. Simply icing your knee can assist with the inflammation and relieve a great deal of the pain. In cases of chronic tendonitis, heat may be more useful in decreasing pain. Your physical therapist may also use electrical modalities such as ultrasound or interferential current to help decrease the pain and control the amount of inflammation. Some mild inflammation is actually needed in order for the injury to heal. Massage, especially for the quadriceps muscle, may also be helpful.
Medication to ease the pain or inflammation can often be very beneficial in the overall treatment of quadriceps tendonitis. Your physical therapist may suggest you see your doctor to discuss the use of anti-inflammatories or pain-relieving medications in conjunction with your physical therapy treatment. Your physical therapist may even liaise directly with your doctor to obtain their advice on the use of medication in your individual case.
As inflammation of the quadriceps tendon most often occurs due to repetitive activity, rest is an important part of the treatment. ‘Relative rest’ is a term used to describe a process of rest-to-recovery based on the severity of symptoms. If you are experiencing pain while doing nothing (resting) it means the injury is more severe and your physical therapist will advise a period of strict rest and possibly even a short time of immobilization in a splint or brace to prevent any repetitive knee flexion/extension. When pain is no longer present at rest, then a gradual increase in activity is permitted so long as there is no return in resting pain.
Once the initial pain and inflammation has calmed down, your physical therapist will focus on improving the flexibility, strength, and alignment around the knee joint and the entire lower extremity. Static stretches to increase the flexibility of the muscles and tissues around the knee (particularly the quadriceps and iliotibial band on the outside of the knee) will be prescribed by your physical therapist early on in your treatment. Again, any tightness in the muscles or tissues around the knee can increase the pull on the quadriceps tendon or affect alignment during walking, running or jumping so it is important to address this immediately. Dynamic stretching (rapid motions that stretch the tissues quickly) will also be taught and will be incorporated into your rehabilitation exercise routine as part of your warm-up once you return to doing more aggressive physical activity. Dynamic stretches are used to prepare the tissues for activity whereas static stretches focus more on gaining flexibility.
Strength imbalances will also affect the alignment of the knee and can cause muscles to tighten. Your physical therapist will determine which muscles in your individual case require the most strengthening. Strength in both the knee and the hip (which controls the knee position) are very important. When bending the knee, the quadriceps tendon is placed under load while it is stretching. This load can be tremendous especially when jumping or landing. In order to prepare the healing tendon to take this load, your physical therapist will prescribe ‘eccentric’ muscle strengthening. Eccentric contractions occur as the muscle lengthens and the tendon is put under stretch. Bending your knee quickly into a squatting position and then stopping rapidly (drop squats) encourages the knee to adapt to the force that will eventually be needed to return to physical activity. When appropriate, weights can be added to simulate the increased body weight that the knee endures during running and jumping. Your physical therapist may even ask you to do this exercise on a board slanting downwards (approximately 25 degrees) which has been shown to also increase the force through the tendon. In addition, an electrical muscle stimulator on the quadriceps may be used which encourages improved recruitment of the quadriceps muscle. All exercises should be completed with minimal or no pain and advancing the exercises should be done at the discretion of your physical therapist as not to flare up the healing tendon.
In addition to stretching and strengthening the knee, bracing or taping the patella or the quadriceps tendon itself can help you do exercises and activities with less pain. Your physical therapist can educate you on which brace would be most appropriate for you. Most braces for knee tendonitis problems are made of soft fabric, such as cloth or neoprene. These braces work by encouraging proper alignment of the patella in the femoral groove and/or by distributing the force on the quadriceps tendon which is, in turn, improves the functioning of the quadriceps mechanism. An alternative to bracing is the use of tape. Your physical therapist can tape your knee for you and can also teach you how to do it for yourself. Taping is an easy and cost-effective way to determine if a brace will decrease your pain before actually investing in one. Patients commonly report less pain and improved function with both taping and bracing.
Proper alignment of your entire lower extremity is paramount to decreasing the overall stress that is placed on your quadriceps tendon. In addition to strengthening and stretching, foot orthotics may be useful to correct your foot position, which encourages proper alignment up the lower extremity chain. Your physical therapist can advise you on whether orthotics would be useful for you, and also on where to purchase them.
A critical part of our treatment for quadriceps tendonitis at In Motion Therapy includes education on returning to physical activity. Bending and straightening your knee occurs often even in everyday activities such as walking or stair climbing so a quadriceps tendon that is recovering from injury can easily be re-aggravated. Returning to your normal physical activity at a graduated pace is crucial to avoid repetitive tendonitis pain or a chronic injury. Advice from your physical therapist on the acceptable level of activity at each stage of your rehabilitation process will be invaluable, and will assist you in returning to your activities as quickly but as safely as possible.
With a well-planned rehabilitation program, adherence to suggested levels of rest and activity modification, and by addressing the intrinsic and extrinsic factors that are modifiable, most patients are able to return to their previous level of activity without recurring symptoms. If, however, your pain continues and does not respond to conservative treatment, your physical therapist may refer you back to your doctor or to an orthopaedic surgeon so you may discuss whether surgery may be an option for treatment.
In Motion Therapy provides services for physical therapy in Duluth.
Surgery
Surgery is rarely needed for quadriceps tendonitis. If nonsurgical treatment fails to improve your condition, however, then surgery may be suggested. Surgery is designed to stimulate healing through revascularization (restoring blood supply). More severe cases may require the attachment of the quadriceps tendon to be moved in order to alter the biomechanics of the quadriceps mechanism. During the surgical procedure weak, damaged tissue is removed and any injured tendon is also repaired.
Arthroscopic revascularization procedures can usually be done on an outpatient basis (you can leave the hospital the same day.) If your problem requires a more involved surgical procedure such as moving the quadriceps tendon attachment, you may need to spend one or two nights in the hospital.
Post Surgical Rehabilitation
What should I expect after treatment?
Patients will benefit greatly from partaking in physical therapy at In Motion Therapy after quadriceps tendon surgery. More involved surgeries for patellar realignment or restorative procedures for tendon tissue usually require a delay before starting therapy in order to give the tissues a short time to begin the healing process before they are stressed. Rehabilitation will also be slower with a more involved surgery, as more time is needed to allow the tendon to heal even more before too much strain is put on the knee. Your surgeon may want you to wear a brace for the initial period after your surgery to protect the knee. Once rehabilitation begins, you will be able to remove the brace to do your exercises while you are at the clinic and when you are at home. Complete removal of the brace will be dictated by your surgeon and physical therapist, and will occur once your thigh muscles are strong enough to support the leg, and once your reaction time is quick enough to protect the knee if you should slip.
Your first few appointments at In Motion Therapy after surgery will focus on controlling the pain and swelling from the surgery. Icing the knee frequently will assist with the inflammation and relieve a great deal of the pain. Your physical therapist may also use electrical modalities such as ultrasound or interferential current to decrease the pain and inflammation. Massage, particularly for the quadriceps muscle, may also be helpful in the early stages post-surgically.
One of the first exercises your physical therapist will prescribe will be some gentle range of motion exercises for your knee to gradually regain full movement. This should be done within a pain-free range of motion, however, movement will be encouraged even if it causes a slight bit of discomfort as the movement itself can greatly assist with dispersing any inflammation as well as improving the overall level of pain. A stationary bicycle can be very useful in the initial stages of gaining range of motion in the knee, so if able, you will be encouraged to use one. Even if you are unable to fully rotate the pedals, the back and forth motion on the bike is an excellent method of slowly encouraging the knee to regain its full range of bending and straightening.
When appropriate your physical therapist will begin to add some gentle strengthening exercises for your knee. Initially these may only involve isometric exercises, where you tighten and hold the quadriceps muscle without actually moving the knee itself. Isometric exercises can be done almost immediately within the limits of discomfort. A muscle stimulator may be used on the quadriceps at this point to encourage the muscle fibers to contract. Gradually your therapist will advance your strengthening exercises.
The more advanced exercises will address any deficits in strength that your physical therapist has identified as a contributing factor to the initial development of your quadriceps tendonitis.
As you recover from the direct effects of the surgery, your physical therapist will begin to add in similar exercises to your program as those listed under non-surgical rehabilitation. Flexibility of the knee and hip will be addressed, as well as the strength, and the overall alignment of these joints during your rehabilitation exercises and everyday activities. Eccentric exercises will be added as soon as they are appropriate, and exercises specific to the sport you enjoy will also be incorporated as soon as it is safe to do so
When you are well under way with your rehabilitation, regular visits to In Motion Therapy will end. Your physical therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program. Generally, rehabilitation at In Motion Therapy after surgery for quadriceps tendonitis goes extremely well and clients can return without difficulties to the activities they enjoy participating in. If however, your pain is lasting longer that your therapist thinks it should or you are not progressing as rapidly as they would expect, your therapist will ask you to follow up with your surgeon to ensure that there are no complicating factors impeding your rehabilitation.
Portions of this document copyright MMG, LLC.
In Motion Therapy provides services for physical therapy in Duluth.
 Alignment or overuse problems of the knee structures can lead to strain, irritation, and/or injury of the quadriceps muscle and tendon. This produces pain, weakness, and swelling of the knee joint.
Alignment or overuse problems of the knee structures can lead to strain, irritation, and/or injury of the quadriceps muscle and tendon. This produces pain, weakness, and swelling of the knee joint.

 The patella (kneecap) is the moveable bone on the front of the knee. This unique bone is wrapped inside a tendon that connects the large muscles on the front of the thigh, the quadriceps muscles, to the lower leg bone.
The patella (kneecap) is the moveable bone on the front of the knee. This unique bone is wrapped inside a tendon that connects the large muscles on the front of the thigh, the quadriceps muscles, to the lower leg bone.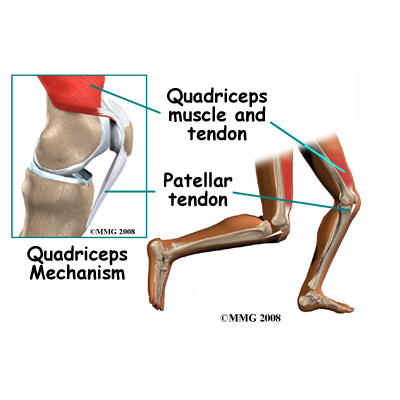
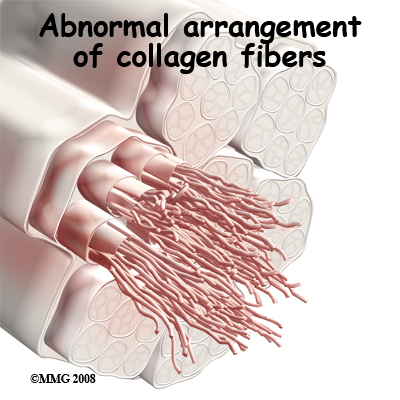 Strength of the patellar tendon is in direct proportion to the number, size, and orientation of the collagen fibers that make up the tendon. Overuse is simply a mismatch between load or stress on the tendon and the ability of that tendon to distribute the force. If the forces placed on the tendon are greater than the strength of the structure, then injury can occur. Repeated microtrauma at the musculotendinous junction may overcome the tendon's ability to heal itself. As a result issue breakdown occurs triggering an inflammatory response that leads to tendonitis and even partial tears.
Strength of the patellar tendon is in direct proportion to the number, size, and orientation of the collagen fibers that make up the tendon. Overuse is simply a mismatch between load or stress on the tendon and the ability of that tendon to distribute the force. If the forces placed on the tendon are greater than the strength of the structure, then injury can occur. Repeated microtrauma at the musculotendinous junction may overcome the tendon's ability to heal itself. As a result issue breakdown occurs triggering an inflammatory response that leads to tendonitis and even partial tears.