Introduction
Welcome to In Motion Therapy's information guide about Platelet-Rich Plasma Treatment of Musculoskeletal Problems.
Platelet-rich plasma (PRP) (also known as blood injection therapy)) is a medical treatment being used for a wide range of musculoskeletal problems. Platelet-rich plasma refers to a sample of serum (blood) plasma that has as much as four times more than the normal amount of platelets. Platelets are the smallest cells in the blood and are essential for blood clotting and injury healing. PRP treatment enhances the body’s natural ability to heal itself and is used to improve healing and shorten recovery time from acute and chronic soft tissue injuries.
PRP injections have been used for years after plastic surgery and surgery on the mouth, jaw, and neck. It seems to promote bone graft healing. Researchers have found a way to combine this substance with other chemicals to make it into a putty or gel that can be painted on a surgical site to speed up healing.
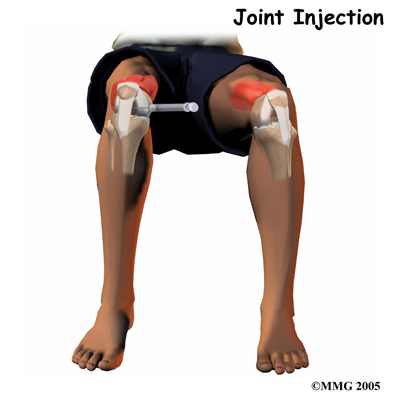
Blood injection therapy of this type has now been used for knee osteoarthritis, degenerative cartilage, spinal fusion, bone fractures that don’t heal, and poor wound healing. This treatment technique is fairly new in the sports medicine treatment of musculoskeletal problems, but is gaining popularity quickly.
This guide will help you understand:
- what your doctor hopes to achieve
- who can benefit from this procedure
- what happens during the procedure
- what to expect as you recover
- what In Motion Therapy’s approach to rehabilitation is
Anatomy
Platelets are part of the blood that circulate around the body ready to help with blood clotting should you have a cut, broken bone, injury that bleeds internally, or any other type of injury. Besides containing clotting factors, the platelets release growth factors that help start the healing sequence. With a concentrated amount of platelets, larger quantities of these growth factors are released to stimulate a natural healing response. Plasma is the clear portion of the blood in which all the other blood particles such as platelets, red blood cells, and white blood cells travel.
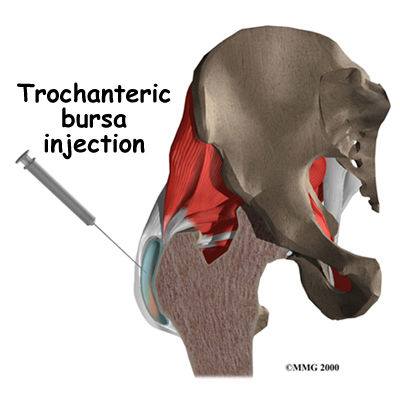
In theory, blood injection therapy could be used in any area where a rapid healing response is desired such as the tendon-muscle junction, muscle injuries, torn ligaments, damaged joints, or inflamed tissue (e.g., plantar fasciitis). PRP treatment might also be used on the skin where delayed wound healing has created a site open to infection or for a pressure ulcer that is open and draining. Patients with non-healing ulcers from poor circulation related to diabetes, paralysis, immobility, and chronic neurologic disorders may be able to receive gel PRP treatments to achieve healing.
 In regards to its use in sports therapy, PRP can play a significant role in treating injuries to tendons and ligaments. These tissues don’t always heal well because both of them have a poor blood supply. Connective tissues such as ligaments and tendons heal by filling in with scar tissue that doesn’t bear the brunt of large loads well. This increases the risk of re-injury. Chronic tendon injuries are related to degeneration in the tendon tissue, which doesn’t always respond well to traditional forms of therapy as these therapies do not necessarily improve the tendon’s ability to create new tissue and heal in the same way that PRP does. In addition, injections of PRP don’t have the side effects that can occur with other treatments such as steroid injections or long-term use of non-steroidal anti-inflammatory drugs (NSAIDs).
In regards to its use in sports therapy, PRP can play a significant role in treating injuries to tendons and ligaments. These tissues don’t always heal well because both of them have a poor blood supply. Connective tissues such as ligaments and tendons heal by filling in with scar tissue that doesn’t bear the brunt of large loads well. This increases the risk of re-injury. Chronic tendon injuries are related to degeneration in the tendon tissue, which doesn’t always respond well to traditional forms of therapy as these therapies do not necessarily improve the tendon’s ability to create new tissue and heal in the same way that PRP does. In addition, injections of PRP don’t have the side effects that can occur with other treatments such as steroid injections or long-term use of non-steroidal anti-inflammatory drugs (NSAIDs).
Since the early 1990s, plasma-rich platelets have been injected into non-healing tendon tears, fibrosed (scarred) tendons, and osteoarthritic knees. As the growth factors released by the platelets can stimulate bone mineralization, platelet-rich plasma may help a break in a bone that isn’t healing. It has also been used with bone grafts to help expedite spinal fusion.
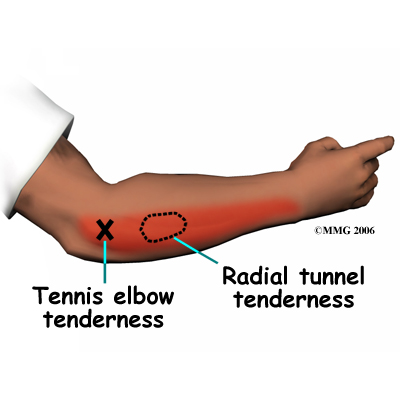
Patients with chronic tendinitis (e.g., tennis elbow, patellar tendinitis or jumper’s knee, Achilles tendinitis) have also benefited from this treatment. It’s even being tried on hernias, labral (shoulder cartilage) tears, meniscal tears of the knee, and ankle sprains. Some surgeons are using it more and more with any orthopedic surgery involving the soft tissues to augment (reinforce) bone or ligamentous graft materials already being used.
Rationale
What do doctors hope to achieve with this treatment?
 The main purpose of PRP injections is to foster healing where it has not otherwise occurred (in a chronic or non-healing injury) or to speed up healing as in the case of an acute injury. Platelets release bioactive proteins that enhance tissue regeneration and healing. For example, studies show that after using the platelet-rich plasma (PRP) for tendon problems, new tendon cells (called tenocytes) start to develop in the area treated. Chondrocytes (cartilage cells) form when PRP is injected into damaged cartilage. Growth factors that help build new blood supply to the area are also increased in number. At the same time, there is a build up of type I collagen fibers. Type I collagen makes up the base structure of tendon tissue. This healing response may help restore strength faster than normal but long-term studies are needed to prove this and ongoing research continues.
The main purpose of PRP injections is to foster healing where it has not otherwise occurred (in a chronic or non-healing injury) or to speed up healing as in the case of an acute injury. Platelets release bioactive proteins that enhance tissue regeneration and healing. For example, studies show that after using the platelet-rich plasma (PRP) for tendon problems, new tendon cells (called tenocytes) start to develop in the area treated. Chondrocytes (cartilage cells) form when PRP is injected into damaged cartilage. Growth factors that help build new blood supply to the area are also increased in number. At the same time, there is a build up of type I collagen fibers. Type I collagen makes up the base structure of tendon tissue. This healing response may help restore strength faster than normal but long-term studies are needed to prove this and ongoing research continues.
Not everyone with a musculoskeletal problem as described can have this treatment. Anyone with a history of cancer should not have this treatment, nor should women who are pregnant or breast-feeding. If you have a condition called thrombocytopenia (low platelet levels) you should not have PRP injections either. Thrombocytopenia can develop with drug treatment for blood clotting disorders, rheumatoid arthritis, or some forms of chemotherapy for cancer. The use of blood thinners such as Coumadin or Warfarin and the presence of infection in the wound site are also contraindications to using PRP injections.
Preparation
How will I prepare for this procedure?
Most non-surgical procedures (for example when treating tennis elbow, muscle injuries, joint osteoarthritis, or cartilage degeneration) can be done on an outpatient basis, usually in the office setting. When used during surgery, PRP is inserted in the area where the healing needs to be enhanced before the wound is closed. For example, it may be injected to enhance ligament or tendon repairs in such procedures as anterior cruciate ligament (ACL) reconstruction, rotator cuff repairs, or Achilles tendon repairs.
Treatment with PRP is broken down into two steps: preparing the platelet-rich plasma for injection and then injection into the affected area. First, blood is drawn from your arm, put into a test tube, and is then used to create the injected fluid. The test tube itself is placed in a machine called a centrifuge. The centrifuge spins the blood fast enough to separate it into layers based on weight. Heavier parts (e.g., red blood cells) stay on the bottom. Platelets and white blood cells spin out just above the red blood cell layer. Lighter particles (plasma without platelets or blood cells) make up the top layer in the test tube.
Once you have had your blood drawn, the sample is prepared right away. You can have the injection as quickly as 30 minutes later.
The Procedure
What happens during the procedure?
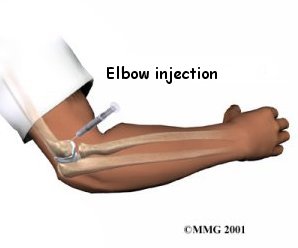
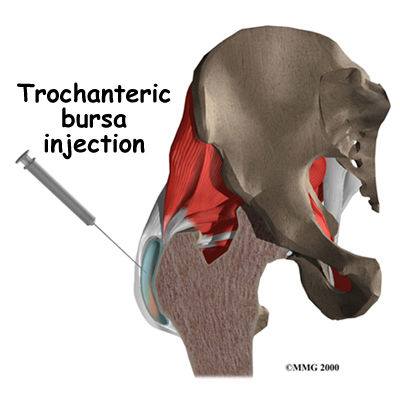
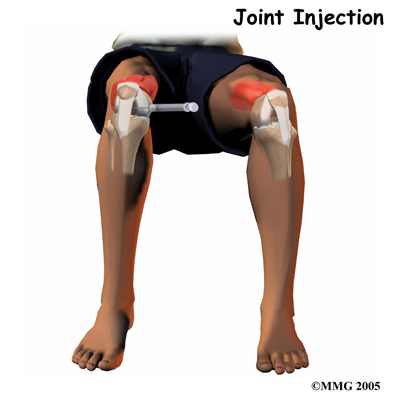
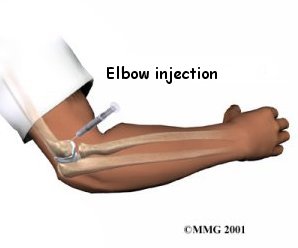
Nonsurgical Treatment
Once the PRP has been prepared, it is injected into the damaged area (e.g., tendon, muscle, cartilage, joint, bone). The surgeon may use imaging such as fluoroscopy (real-time, 3-D X-rays) or dynamic musculoskeletal ultrasound to place the needle that delivers the PRP directly into the joint or other area of injury. You will not be asleep or anesthetized unless the plasma is applied during a surgical procedure. When used on an outpatient basis for a nonsurgical treatment, a numbing agent (e.g., novocaine, lidocaine, marcaine) is used so that you don’t feel anything around the injection area.
Surgery
For open incisions or arthroscopic surgeries, such as labral repairs, meniscal repairs, and tendon or ligament repairs, the PRP is placed around the anchors and sutures holding the soft tissues together. Tiny clots form quickly. The surgeon then ties the sutures down reducing the tear, and thus trapping the PRP clot in the repair site.
Early attempts to use this procedure contained four times the normal amount of platelets but surgeons have found they can use far less than that to achieve the same result. Scientists are still actively studying the best way to use this treatment. It’s not clear yet just how much PRP is needed to get the best healing response. The optimal number of injections needed and the time frame between injections also remain yet to be determined. In studies done so far, one to three injections have been used with one to two weeks between injections.
Complications
What might go wrong?
Research regarding this procedure is still underway in a number of clinics with a wide range of patient problems. There have been, however, very few reports of complications or adverse reactions. This being said, whenever an injection of any kind is given, there is always the risk of infection. In addition, some patients have reported increased pain, redness, and swelling at the injection site but this response didn’t last long.
Since you donate your own blood to use in the procedure there is little concern about reactions to the blood, transfer of infection, HIV, or cancer cells through someone else’s blood. Donor blood products might be used for individuals with medical issues that prevent them from donating their own blood. In these cases, donated blood is carefully screened, so again, the risk of infection or reaction to the blood is very low. Rarely the needle may go through a blood vessel or nerve causing bleeding or nerve damage.
With other types of injection treatment, scar tissue and calcification (formation of tiny calcium deposits) can occur around the injection site. This has not been reported with PRP injections, but it is theoretically possible. Also possible, but uncommon, are allergic reactions to the lidocaine or marcaine used as a numbing agent.
More often the worst consequence is that you won’t get any better with the treatment.
After the Procedure
What happens after the procedure?
Nonsurgical
Immediately after the procedure, you will remain lying down and under observation for a few minutes up to 30 minutes. You might have some discomfort in the area of the injection that can last a few days or up to a week. Sometimes it can seem like your injury is worse than before the treatment, but that is because an inflammatory response has just been stimulated. This is common, and the temporary worsening of your symptoms usually doesn’t last.
Once you return home, you can use ice over the injected area for pain relief, elevate the leg or arm, and limit your activities as much as needed to remain comfortable. Your doctor may suggest using Tylenol for pain relief but ibuprofen or other anti-inflammatories are not advised as the treatment is designed to set up an inflammatory response, so you don’t want to stop that process with medications. Some doctors will recommend avoiding heavy or repetitive physical activity with the treated body part for up to a week to allow the healing to occur.
After Surgery
Protocols after surgery where PRP injection was used vary considerably based on the type of surgery performed. Your surgeon will advise you on how best to care for your injury to maximize healing and avoid complications.
Rehabilitation
What should I expect as I recover?
The most surprising aspect of recovery after treatment with platelet-rich plasma is the speed of recovery. For example, some high-level athletes have found that they could return to full sports participation and competitive play in half the time expected for acute tendon injuries and with no negative side effects and minimal scar tissue or adhesions. The majority of patients report being pain free. Patients have also reported using less pain medication, and gaining greater joint motion over a shorter period of time. Overall, patients get back to regular daily activities with greater speed and ease.
Treatment from a physical therapist at In Motion Therapy after PRP injections will help you regain motion, strength, motor control, and function of your injected area. Physical therapy can begin as soon as your doctor allows. As research is still ongoing into this treatment, there isn’t a standard proven rehabilitation program to follow yet. Your doctor will decide, based on your individual injury and his or her clinical experience when the best time after the injection is to start rehabilitation. Your physical therapist at In Motion Therapy will liaise closely with your doctor to ensure you return to activity as soon as possible without disturbing the healing process initiated by the PRP injection.
If you have any residual excessive pain after the injection your physical therapist may use modalities such as ultrasound, interferential current, or ice or heat to assist with this pain. Massage around the area may also be used although direct deep massage over the healing injury is generally avoided so as not to disturb the healing process. Again, the idea is to allow inflammation to occur (in a controlled fashion) so excessive use of modalities for the purpose of reducing inflammation will be avoided.
As your doctor allows, your physical therapist will teach you stretching and strengthening exercises to be done in the clinic and as part of a home exercise program. Gentle stretching for the muscles around the injected area can usually be started nearly immediately after the injection; however, strengthening exercises and other forms of exercise involving the area will not begin immediately as the tissue requires healing time after the injection before being heavily stressed. Again, time frames recommended prior to strengthening can vary depending on many variables including the number of injections and the time between these injections. In some programs where PRP injections have been used for tendon problems, patients were allowed to do light activities after a second injection given 15 days after the first injection. Strengthening exercises were started after a third (and final) injection given 15 days after the second injection. In all cases, strengthening exercises will be progressed by your physical therapist at In Motion Therapy as soon as your doctor allows. These exercises may include the use of light-weights or Theraband for added resistance. As the healing process progresses, eccentric exercises will be added. Eccentric exercises are those that force the healing tissue to bear weight while the tissue is lengthening or in a lengthened position. These exercises are particularly important in preparing the healing tissues to withstand the rapid motions encountered in everyday life and sport such as lifting a bag, throwing, running, or jumping. For example, an eccentric exercise after an achilles tendon PRP injection would be a calf raise on a stair followed by a rapid drop back down into a stretched calf position. As rehabilitation progresses, jumping from a height would be incorporated.
Proprioception exercises will also be an important part of your rehabilitation at In Motion Therapy. Proprioception is the ability to know where your joint or limb is in space without looking at it. Injury to any area can decrease the functioning of the receptors that assist with proprioception. Injury to a joint or the tendons that attach close to the joint are particularly sensitive to a decline in proprioceptive function. Exercises that incorporate balance (standing on one foot for the lower extremity) or those requiring precision (throwing a ball at a target for the upper extremity) will challenge your proprioception and assist in maximizing the function of your injured area so you can return to high level activities.
Avoiding unnecessary stress to the area will also prevent re-injury. For this reason, your physical therapist will also look closely at your body alignment and how you use the injured area in everyday tasks such as using the computer or climbing stairs to ensure unnecessary stress is not added to your body. Proper alignment and good technique with all your rehabilitation exercises will also be emphasized for this same reason.
A critical part of our treatment for any injury at In Motion Therapy includes education on the appropriate time to return fully to the physical activity that you enjoy participating in. For athletes, sport-specific exercises, such as throwing or simulated sport drills will be gradually encouraged as soon as possible to prepare you to return to your desired sport. Others may require education on returning to a full occupational workload or duties of the home such as gardening or housecleaning. For athletes and non-athletes alike your physical therapist will discuss the most appropriate return-to-sport or activity plan for you after a PRP injection and will advise you on the acceptable level of activity at each stage of your rehabilitation process.
Developing optimal tendon healing and muscle strength and then assisting you in returning to your activities as quickly as possible while avoiding any risk of re-injury is the goal of rehabilitation at In Motion Therapy after PRP injections. If a tissue does not re-gain the needed strength after the injection, another injury can occur. By modifying your activities as suggested by your physical therapist, the chance of re-injury will be greatly reduced. With a well-planned rehabilitation program and adherence to suggested levels of rest and activity modification, good success at returning to full activity can be achieved with PRP injections. If however, at any stage, your physical therapist at In Motion Therapy feels that your rehabilitation is not progressing as it should; we will liaise with your doctor to ensure that optimal management of your injury occurs.
Portions of this document copyright MMG, LLC.


 In regards to its use in sports therapy, PRP can play a significant role in treating injuries to tendons and ligaments. These tissues don’t always heal well because both of them have a poor blood supply. Connective tissues such as ligaments and tendons heal by filling in with scar tissue that doesn’t bear the brunt of large loads well. This increases the risk of re-injury. Chronic tendon injuries are related to degeneration in the tendon tissue, which doesn’t always respond well to traditional forms of therapy as these therapies do not necessarily improve the tendon’s ability to create new tissue and heal in the same way that PRP does. In addition, injections of PRP don’t have the side effects that can occur with other treatments such as steroid injections or long-term use of non-steroidal anti-inflammatory drugs (NSAIDs).
In regards to its use in sports therapy, PRP can play a significant role in treating injuries to tendons and ligaments. These tissues don’t always heal well because both of them have a poor blood supply. Connective tissues such as ligaments and tendons heal by filling in with scar tissue that doesn’t bear the brunt of large loads well. This increases the risk of re-injury. Chronic tendon injuries are related to degeneration in the tendon tissue, which doesn’t always respond well to traditional forms of therapy as these therapies do not necessarily improve the tendon’s ability to create new tissue and heal in the same way that PRP does. In addition, injections of PRP don’t have the side effects that can occur with other treatments such as steroid injections or long-term use of non-steroidal anti-inflammatory drugs (NSAIDs).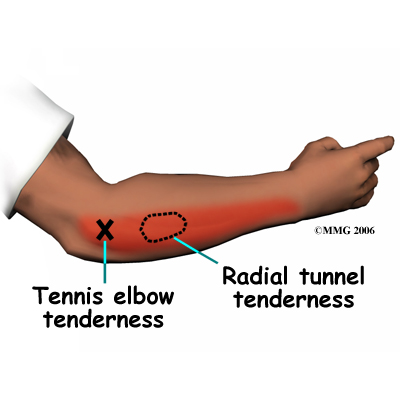 The main purpose of PRP injections is to foster healing where it has not otherwise occurred (in a chronic or non-healing injury) or to speed up healing as in the case of an acute injury. Platelets release bioactive proteins that enhance tissue regeneration and healing. For example, studies show that after using the platelet-rich plasma (PRP) for tendon problems, new tendon cells (called tenocytes) start to develop in the area treated. Chondrocytes (cartilage cells) form when PRP is injected into damaged cartilage. Growth factors that help build new blood supply to the area are also increased in number. At the same time, there is a build up of type I collagen fibers. Type I collagen makes up the base structure of tendon tissue. This healing response may help restore strength faster than normal but long-term studies are needed to prove this and ongoing research continues.
The main purpose of PRP injections is to foster healing where it has not otherwise occurred (in a chronic or non-healing injury) or to speed up healing as in the case of an acute injury. Platelets release bioactive proteins that enhance tissue regeneration and healing. For example, studies show that after using the platelet-rich plasma (PRP) for tendon problems, new tendon cells (called tenocytes) start to develop in the area treated. Chondrocytes (cartilage cells) form when PRP is injected into damaged cartilage. Growth factors that help build new blood supply to the area are also increased in number. At the same time, there is a build up of type I collagen fibers. Type I collagen makes up the base structure of tendon tissue. This healing response may help restore strength faster than normal but long-term studies are needed to prove this and ongoing research continues.